Resources
Types of Urinary Incontinence: Causes, Symptoms, and Solutions
By Lauren Ohayon 10/13/2025
4 Min Read
Let’s be honest – leaking urine is frustrating, inconvenient, and often embarrassing. It’s also far more common than most people realize. While some dismiss it as a minor nuisance or just “part of getting older,” or “that’s how it is after pregnancy”, ignoring urinary leakage can make symptoms worse and more complicated to manage over time.
Incontinence can look different for everyone. For some, it’s a minor leak when sneezing, coughing, or exercising. For others, it’s sudden, uncontrollable urges to urinate that make it difficult to reach the bathroom in time.
The usual advice is to “just do Kegels,” but bladder leaks aren’t always caused by weak pelvic floor muscles alone. In fact, incontinence is often one of the earliest warning signs that something is out of balance in the body’s core system – the coordinated relationship between your pelvic floor, diaphragm, deep abdominals, breath, and your posture.
Table of Contents
What Is Urinary Incontinence?
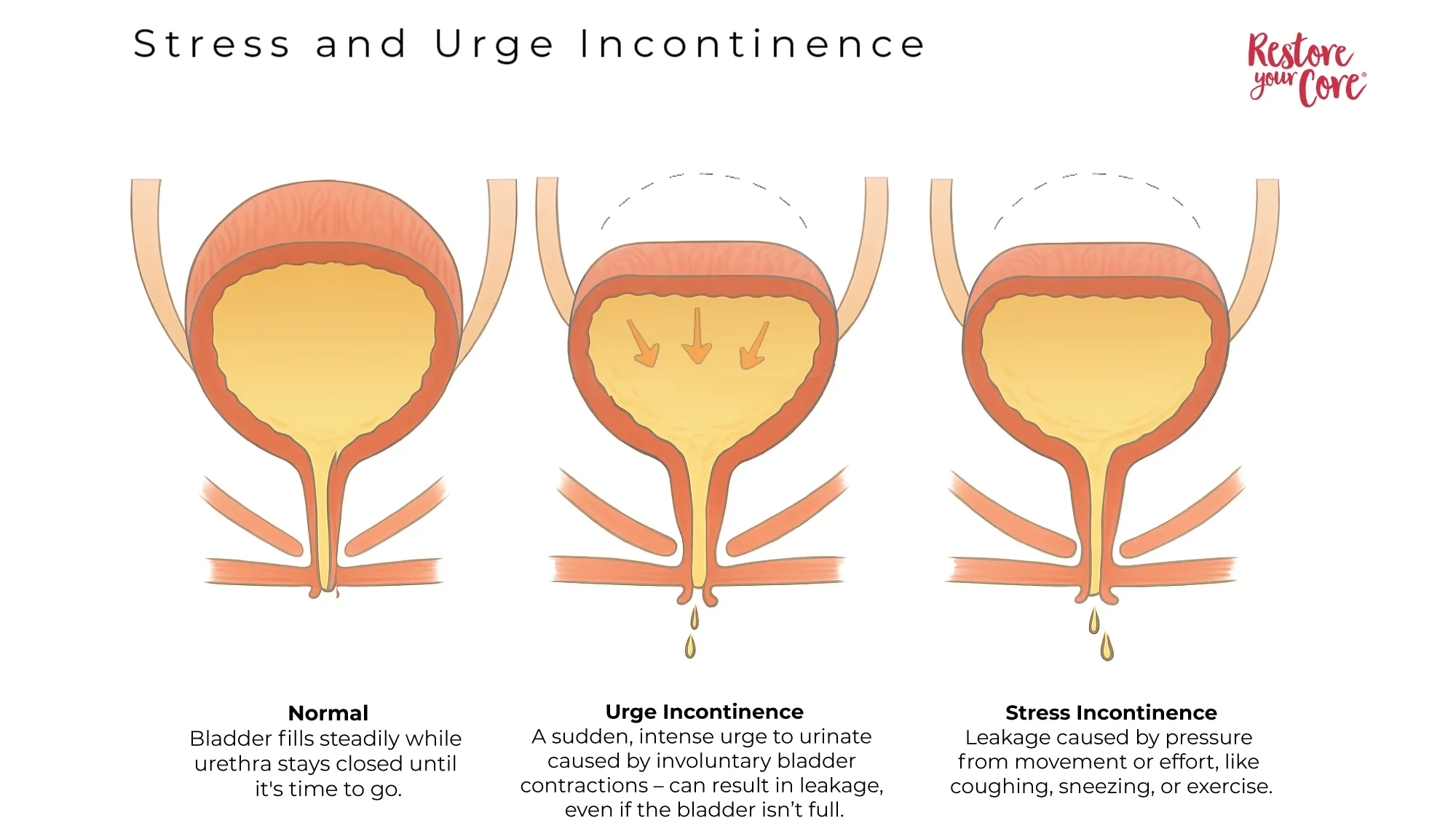
Urinary incontinence is the loss of bladder control, and it affects people in different ways. The most common types of urinary incontinence are stress incontinence and urge incontinence (overactive bladder). Women experience incontinence about twice as often as men, due to anatomical differences as well as the effects of pregnancy, childbirth, and hormonal changes. In fact, one study states that more than 60% of adult women in the United States report some level of urinary incontinence, and about one-third experience leakage at least once a month [1]. However, urinary leakage is not an inevitable part of aging – it’s a sign that something in the body’s system of support and coordination is out of balance.
Understanding the Whole-Body Connection
Incontinence isn’t just about the pelvic floor – it’s about the container the pelvic floor lives in: your whole body. Focusing only on Kegels treats the symptom, not the underlying cause. Just like a foot injury can eventually cause pain in the knee, hip, and back, bladder leakage may reflect imbalances that start outside the pelvic floor itself. Addressing the root cause requires a whole-body approach.
Symptoms of Urinary Incontinence
Some of the most common symptoms of bladder incontinence are:
- Leaking urine during exercise, lifting, bending, running or jumping
- Leaking when you cough, sneeze, or laugh
- Sudden and intense urge to urinate
- Urinating in your sleep
- Difficulty making it to the restroom in time
These symptoms can vary in severity and frequency. Some people experience occasional, minor leaks, while others deal with more significant episodes that significantly impact their quality of life. Understanding your specific symptoms helps identify which type of urinary incontinence you’re experiencing and guides appropriate treatment.
Types of Urinary Incontinence
The most common types of incontinence include:
| Type | Main Trigger | Most Common In |
| Stress | Coughing, sneezing, jumping, lifting | Pregnancy, post-natal, athletes |
| Urge (overactive bladder) | Sudden intense urge to urinate | Older adults, hormonal fluctuations, pregnancy, irritating food and drink |
| Overflow | Incomplete bladder emptying | Enlarged prostate, nerve damage |
| Functional | Physical/cognitive barriers | Mobility or cognitive issues |
| Mixed | Combination of stress and urge incontinence | Varies |
Stress Urinary Incontinence
More common in pregnancy or those who delivered vaginally. May be triggered by coughing, laughing, bending, lifting, jumping, or sneezing. Stress urinary incontinence treatment needs to address the whole pressure management system, not just isolated muscle strength in the pelvic floor.
Urge Urinary Incontinence
More often, an issue with aging is characterized by increased urinary frequency and urgency (overactive bladder). This type creates a sudden, overwhelming need to urinate that is difficult to control.
Overflow Incontinence
Overflow incontinence is characterized by dribbling urine, increased frequency of urination, and an inability or feeling of incompleteness after urinating.
Functional Urinary Incontinence
Functional urinary incontinence occurs when physical limitations, cognitive issues, or environmental barriers prevent reaching the bathroom in time, despite normal bladder function. This might include mobility problems, dementia, or inaccessible bathrooms.
Mixed Incontinence
It is possible to experience a combination of the symptoms and types mentioned above, most commonly stress and urge together.
Causes of Urinary Incontinence Explained
Urinary incontinence can happen for various reasons. However, it is not always a sign of something severely wrong. Often, the case may be related to changes your body undergoes during or post-pregnancy or imbalances within your body.
Some of the more common urinary incontinence causes include:
Pregnancy: Hormonal shifts, as well as your growing baby, adding pressure to your bladder and pelvic floor, may lead to incontinence. Studies show that 39.5% of pregnant women experience urinary incontinence, especially in the third trimester, with vaginal delivery increasing postpartum risk [2].
Childbirth: A vaginal delivery may weaken the muscles required to control urination as well as lead to other issues, such as pelvic organ prolapse. Urinary incontinence after childbirth is incredibly common but very treatable.
Aging: Although incontinence is not a normal part of aging, the muscles may become weaker, and bladder contractions may become more frequent as you get older.
Menopause: During menopause, declining hormones and other physical changes can affect the muscles required for bladder control.
Hysterectomy: A woman’s uterus and bladder depend on many of the same muscles, ligaments, and structures for support. Any surgical procedure that may involve or compromise a woman’s reproductive system may damage the pelvic floor and supporting muscles and ligaments, which can lead to incontinence.
Enlarged prostate: In men, an enlarged prostate can lead to male incontinence.
Treatment for Urinary Incontinence: Non-Surgical Approaches
Exercise and movement protocols have helped many people find relief from urinary leakage and regain bladder control.
Conservative First-Line Treatment
These urinary incontinence treatments prove highly effective:
- Targeted exercise programs addressing whole-body patterns
- Bladder training and timed voiding
- Lifestyle modifications
- Pelvic floor physical therapy
Medical Interventions (When Necessary)
While movement-based solutions work for stress and urge incontinence, some situations benefit from additional support:
Pessary for Urinary Incontinence
A removable device placed in the vagina to support pelvic organs. It’s particularly helpful for those with prolapse-related incontinence and can be used in conjunction with strengthening exercises.
Medications
Various drugs can help with urge incontinence by calming bladder muscles or improving urethral closure. However, side effects often make them less desirable than exercise-based approaches.
Surgery
Reserved for severe cases unresponsive to conservative treatment of urinary incontinence after at least 6-12 months of consistent effort. Options include slings, bladder neck suspension, and other procedures.
Effective Exercises for Urinary Incontinence
Exercises for Incontinence Urinary Relief You Can Start Today
Below are exercises I teach in my pelvic floor program, Restore Your Core®, to help control the flow of urine.
Core Engagement (Foundation for All Movements):
- Lie on your back with your knees bent and feet flat on the floor.
- Inhale deeply through your nose, expanding the ribs.
- Exhale slowly through your mouth, imagining you’re blowing out 100 candles on a birthday cake.
- Focus on making the exhale longer than the inhale, promoting relaxation and feeling your core respond.
- Repeat the inhale-exhale cycle for several breaths.
This can and should be practiced whenever working out and managing a load, a weight, or a core move. This helps the core to be reflexive and promotes optimal engagement as your core responds to your breathing.
Seated Side Bend:
- Sit in a chair or kneel if that feels more comfortable. Consider sitting on a block or some pillows to keep your spine in neutral.
- Hold a yoga strap or belt overhead. Bend your elbows slightly to take the stress off your neck and shoulders.
- Exhale, blow candles (as above), and side bend to the right, squeezing your ribs towards your pelvis. Return to the center, then exhale and bend to the left side.
- Your core should not bulge, brace or push out as you do these.
These are great for upper body mobility, torso length and strength and are a great way to work your core without strain.
Cat Cow:
- Begin on your hands and knees, line up your wrists underneath your shoulders and your knees underneath your hips.
- Exhale as you round your spine, tucking your chin to your chest and drawing your tailbone under, rounding your entire back.
- Feel the stretch along your spine, especially in the lower back, as you tuck your pelvis under you.
- On an inhale, push your hands into the floor and “as if” drag them towards your knees as you lift your chest up, feeling the contraction in the upper back. And a stretch across the front of your chest.
- Exhale for Cat (rounded back) and inhale for Cow (arched back).
- Flow between Cat and Cow, coordinating your breath with each movement.
- Repeat the flowing movement for several breaths, moving at a pace that feels comfortable for you.

Pelvic Clock:
- Lie on your back with your knees bent and your feet flat on the floor.
- Imagine that your belly button is 12 o’clock and your pubic bone is 6 o’clock, and there is a straight line between the two.
- Using small movements with your pelvis only, tuck and untuck your pelvis as you trace that straight line between 12 o’clock and 6 o’clock.
- Ideally, you should be able to generate movement from your pelvis, rather than pushing into your feet.
- Repeat 8 times, then start to recruit your feet and other muscles, making the movement larger.
- Repeat this larger movement 8 times, then go back to the quiet movement of your pelvis only 8 times.
- Now move on to 3 o’clock to 9 o’clock – side-to-side movement in your pelvis.
- Try to keep your knees still; they might want to sway from side to side like windshield wipers, but try to keep them quiet.
- After 8 rounds, make the movement bigger and allow your knees to follow along.
- Then go back to 8 more rounds of just the pelvis moving.
- From here, you can explore moving slowly, trying to touch all the numbers on the clock.
- Now try it counter-clockwise.
Notice which movements were easier, or if any of them felt sticky or hard to access. This is a great way to mobilize the pelvis, and it’s incredible for your pelvic floor.
Wide Leg Stretch:
- You may need a chair or stool for this movement.
- Face the stool and open your legs wide.
- Bend forward from your hips, keeping your spine long (don’t round or arch your back).
- Place your hands on the stool, blocks, or floor – whichever allows you to keep your spine in neutral.
- Shift your hips to the right; your right hip will lift higher. Feel free to bend your right knee if you are doing this movement for the first time.
- Pause and enjoy the deep groin stretch on the left side.
- Now shift your hips to the left and sink into the stretch on this side.
- Move from side to side, staying for a few breaths on each side and feeling that deep stretch.
- Your hips should hike up and down rather than moving from side to side – ensure it’s a hip joint movement.
Wide Leg Stretch and Twist:
- Starting in the same position as the wide leg stretch above.
- Take your right arm and straighten it above your head as you twist your upper body to the right.
- Repeat on the other side.
- Repeat a few times on each side.
Glute Bridge:
- Lie on your back, knees bent, and feet flat on the floor.
- Tuck your pubic bone gently toward your belly button, flattening your lower back to the floor.
- Push your feet into the floor to lift your pelvis slowly while maintaining the tuck in your pelvis.
- Keep your ribs on the floor, focusing on feeling the exercise in your glutes.
- Repeat 6-8 times.
Remember to start every movement with candles exhale
Kegel Exercises for Urinary Incontinence: Are They Enough?
While Kegel exercises for urinary incontinence are commonly recommended for strengthening pelvic floor muscles, urinary incontinence (like other symptoms of pelvic floor dysfunction) is often a whole-body issue. A comprehensive approach, including mindful strengthening and mobility exercises, relaxation techniques, and improved breathing mechanics, provides more effective long-term solutions. If your pelvic floor is already tight, Kegels can often exacerbate the issue.
When to Seek Medical Advice
While urinary incontinence can usually be treated effectively with exercises like those suggested above, there are some circumstances when a professional assessment is required.
If you find yourself experiencing more frequent episodes of urinary leakage or losing a higher volume of urine, please seek medical advice from your primary healthcare provider.
If you get to a stage where your urinary incontinence is seriously affecting the quality of your day-to-day life and stopping you from taking part in your normal activities – it’s time to see a doctor.
Red Flags That Require Immediate Medical Attention:
- Blood in urine
- Complete inability to urinate
- Severe pelvic pain
- Signs of infection (fever, unusual discharge)
- Sudden onset of severe incontinence
- Pain during urination

Prevention Tips for a Leak-Free Life
You can help prevent urinary incontinence by adopting proactive measures to support your bladder and general health. Here are some tips and exercises aimed at preventing leak pee:
- Maintain a Healthy Weight: Carrying excess weight can strain pelvic floor muscles, contributing to urinary incontinence. Adopting a balanced diet and engaging in regular physical activity can help maintain a healthy weight, reducing the risk of bladder issues.
- Stay Hydrated: While it may seem counterintuitive, staying adequately hydrated is crucial for bladder health. Dehydration can irritate the bladder and exacerbate incontinence. Aim for consistent water intake throughout the day to support overall urinary function.
- Avoid Bladder Irritants: Certain foods and beverages can irritate the bladder, leading to increased urgency and leaks. Limit your intake of alcohol, caffeine, spicy foods, citrus fruits, and carbonated drinks, especially if you notice sensitivity to these items.
- Practice Mindful Movement: Engage in exercises that promote overall body awareness and mindful movement. Our 12-week online program, Restore Your Core® helps to improve posture and muscle tone, and increase balance, positively impacting bladder function.
- Bathroom Habits: Develop healthy bathroom habits by emptying your bladder regularly. Avoid delaying bathroom trips, as holding in urine for extended periods can strain the bladder. Also, avoid going to the bathroom ‘just in case’; this habit can train the bladder to signal the need to go long before it reaches capacity. Create a consistent bathroom schedule to maintain optimal bladder function.
- Pelvic Floor Relaxation Techniques: In addition to strengthening exercises, incorporating relaxation techniques for the pelvic floor is essential. Techniques such as 3D breathing and mindful relaxation can help release tension in the pelvic region, promoting a healthy balance.
By integrating these preventive measures into your lifestyle, you can actively contribute to maintaining a healthy, well-functioning bladder and reduce the risk of urinary incontinence.
Conclusion: You’re Not Alone – and You Can Heal
Urinary incontinence doesn’t mean you’re broken, nor is it permanent. With the right whole-body approach and consistency, you can regain control and confidence. The key is understanding that this is rarely just a pelvic floor issue – it’s about how you move your entire body, and how you manage intra-abdominal pressure.
If you’re ready for a comprehensive solution that addresses the root causes rather than just the symptoms, the Restore Your Core® 12-Week Program’s structured and progressive approach has helped thousands overcome urinary incontinence. You deserve to live without fear of leaking.
FAQs
What are the different types of urinary incontinence?
The main types of urinary incontinence include stress incontinence (leaking with coughing/sneezing), urge incontinence (sudden, intense urgency), overflow incontinence (constant dribbling), functional urinary incontinence (physical barriers to toileting), and mixed incontinence (combination of types) [3].
What causes urinary incontinence?
Urinary incontinence causes include pregnancy, childbirth, aging, pelvic floor tension, hormonal shifts, and surgical procedures such as hysterectomy. It’s essential to address the root causes and consider the holistic aspects of the body rather than focusing solely on pelvic floor symptoms.
What are the common causes of urinary incontinence at night, and how is it different from other nighttime urinary issues?
Urinary incontinence at night can result from overactive bladder, hormonal changes affecting bladder capacity, medications, sleep apnea, or excessive evening fluid intake. It differs from normal nighttime urination (nocturia) as it involves actual loss of bladder control rather than just waking to urinate.
Is surgical intervention necessary for treating urinary incontinence?
In most cases, surgical or medical procedures are unnecessary for treating urinary incontinence and are typically reserved as a last resort. Exercise, along with lifestyle modifications, has helped many individuals find relief from urinary leakage and regain bladder control. However, a professional assessment is recommended if symptoms persist or worsen.
How do you treat stress urinary incontinence naturally?
Natural stress urinary incontinence treatment includes targeted exercises for core and pelvic floor coordination, breathing techniques, posture improvement, and learning proper body mechanics. The RYC® 12-Week Program specifically addresses these whole-body patterns to achieve lasting results.
Are Kegel exercises a good solution for urinary incontinence?
While Kegel exercises are commonly recommended for strengthening pelvic floor muscles, urinary incontinence (as with other symptoms of pelvic floor dysfunction) is often a whole-body issue. A comprehensive approach, including mindful mobility and strengthening exercises, relaxation techniques, and improved breathing mechanics, is a more effective solution.
Is a pessary good for urinary incontinence?
A pessary for urinary incontinence can be helpful, especially when prolapse contributes to symptoms. It provides mechanical support while you work on strengthening and coordinating your pelvic floor muscles.
When should I seek medical advice for urinary incontinence?
If you experience more frequent episodes of urinary leakage, notice a significant increase in urine volume, or experience pain when urinating, it’s advisable to seek medical advice from your primary healthcare provider. Additionally, if urinary incontinence significantly affects your daily life and normal activities, consulting a doctor is recommended.
What is the best online bladder training program?
The Restore Your Core® Method provides a comprehensive, whole-body approach that addresses the underlying causes of non-medical urinary incontinence. The RYC® 12-Week Program is recommended by Medical Doctors, OBGyns, Pelvic Floor Physical Therapists and other Health and Wellness Professionals because it goes beyond traditional bladder training to address the pressure management system of your entire core. Rather than just timing bathroom visits or doing isolated exercises, RYC® teaches you how to retrain your body’s reflexive responses, improve your movement patterns, and build genuine core stability that supports long-term bladder health. With progressive exercises, educational content about your body’s patterns, and support from certified teachers, it provides the structured approach needed for lasting results.
References
[1] Tran, L. N., Reynolds, W. S., & Strope, S. A. (2023). Urinary incontinence. StatPearls.
[2] Rajavuori, A., Karttunen, V., & Andersson, K. (2021). Maternal risk factors of urinary incontinence during pregnancy and postpartum: A systematic review. BMC Pregnancy and Childbirth, 21(1), 588.
[3] Leslie, S. W., Tran, L. N., & Puckett, Y. (2024). Urinary incontinence. In StatPearls. StatPearls Publishing.



