
Understanding Pelvic Organ Prolapse: What You Need to Know
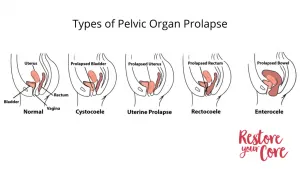
If you’ve recently noticed changes in your pelvic floor health, you’re not alone. Pelvic organ prolapse (POP) affects about 50% of women at some point

If you’ve recently noticed changes in your pelvic floor health, you’re not alone. Pelvic organ prolapse (POP) affects about 50% of women at some point

Are you contemplating hysterectomy? Recently recovering from a hysterectomy? If your doctor hasn’t yet spoken with you about pelvic organ prolapse after hysterectomy, read on
One thing that many of my clients with pelvic organ prolapse ask is, “Can you have intercourse with a prolapsed uterus?” The answer is usually
Childbirth is the primary risk factor for pelvic organ prolapse. While it is impossible to prolapse-proof your birth process, having a better understanding of prolapse

If you’ve recently been diagnosed with pelvic organ prolapse, it’s natural to be overwhelmed by a mix of shock, confusion, fear and even devastation. This
For athletes, especially weightlifters, managing pelvic organ prolapse can be challenging. There are risks to consider before participating in your sport, including the possibility of

The hips and pelvic floor are intimately interconnected muscle systems. A clear understanding of how hip mobility affects the pelvic floor will help you work

Looking for comprehensive guidance on safe and effective exercises designed for the relief and recovery of a prolapsed uterus? Look no further. Learn about what

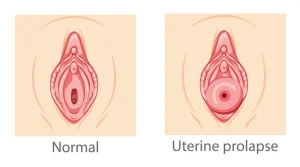
A uterine prolapse occurs when the pelvic floor becomes weakened and the surrounding tissues, muscles, and ligaments are unable to provide proper support to the uterus. This may

What is Rectal Prolapse? Rectal prolapse is another form of pelvic organ prolapse. Rectal prolapse occurs as a result of the rectum (the last part
© 2025 RYC®. All rights reserved.