Rectal Prolapse
4 Min Read
Table of Contents
What is Rectal Prolapse?
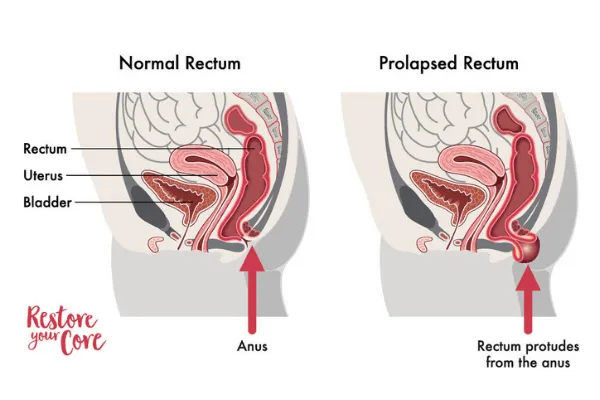
Rectal prolapse is another form of pelvic organ prolapse. Rectal prolapse occurs as a result of the rectum (the last part of the large intestine) being displaced or forced from its normal position. This can lead to the rectum descending or protruding out of the anus.
Rectal prolapse is often more common in older adults, more often in older women, who have experienced prolonged issues with constipation or pelvic floor issues. However, rectal prolapse can affect men and women in various stages of life. Although it is reported to be more common in women postmenopause, it can also occur in people much younger as well.
In this article we will address some of the most pressing questions regarding rectal prolapse and how it may be treated.
Types of Rectal Prolapse
As with other forms of prolapse, rectal prolapse is often a term that defines various stages of a herniated anus. The three types of rectal prolapse include:
- Stage 1: the rectum has become displaced, but does not protrude out of the anal cavity (also know as an internal prolapse)
- Stage 2: the rectal lining begins to descend into the anal cavity
- Stage 3: the rectum extends out of the anus entirely.
In many cases, people have found relief without the need of medical or surgical attention. However, in severe cases, medical attention may be necessary.

Are you looking for safe and restorative exercises to heal from your pelvic floor and core symptoms?
Learn more about the RYC program
Are you looking for safe and restorative exercises to heal from your pelvic floor and core symptoms?
Learn more about the RYC program
Causes of Rectal Prolapse
A rectal prolapse may occur due to various health conditions or as a result of aging. In some cases, it may be a result of complications during pregnancy or injuries to the pelvic or bowel region. Below are a few possible causes of rectal prolapse.
- Chronic constipation or diarrhea: excessive straining during defecation
- Prolonged or chronic history of straining during bowel movements
- Old age: as you grow older, it is common to experience a weakening of the rectal and anal muscles and ligaments. It is also common to experience similar weakening in the pelvic floor, which can create additional weakness in your core.
- Weakening of the anal sphincter
- Injury or past surgical procedures to or near the anal and pelvic regions
- Nerve damage: If the nerves that control your ability to contract the rectum or anus are damaged, rectal prolapse may occur. This can be due to complications during vaginal delivery, paralysis, a spinal injury, lumbar spine surgery, or other surgeries in the pelvic area.
- Other diseases, conditions and infections: There are many other possible causes for rectal prolapse. These can include health conditions such as diabetes, cystic fibrosis, parasitic infections, or other diseases. Or, it may be caused by other corrective surgical procedures, such as a hysterectomy.
Rectal Hernia Symptoms
The most common symptoms of rectal prolapse is the feeling of a bulge or ball extending out of the rectum. This can look like a reddish-colored mass extending outside of the anus, or, in the case of an internal prolapse, feel as if something is stuck in your rectum. These symptoms are often experienced during or after a bowel movement. In many cases, the symptoms will resolve quickly. However, if you have a moderate to severe rectal prolapse, over a prolonged period of time, you may experience the rectum protruding out of the anus at the end of the day. This is often spontaneous and may not require force or straining.
Other symptoms may include:
- Anal pain, pain throughout the rectal tissue
- Rectal bleeding (may appear like a hemorrhoid – swollen blood vessels)
- Fecal incontinence (fecal leakage, leakage of mucus, heavy bleeding)
The symptoms you suffer may change depending on the severity and progression of your prolapse.
Diagnosis
A rectal prolapse requires a proper diagnosis in order to rule out conditions that may correlate. In order for you to receive a proper diagnosis and effective treatment, your doctor will have to perform a rectal exam. Your doctor may ask you to sit on a toilet and attempt to perform a bowel movement in order to see the prolapse.
If your symptoms are varied and severe, there may be a need for more advanced testing in order for your doctor to properly diagnose rectal prolapse. This may help rule out other possible conditions. Below are a few tests your doctor may recommend:
- Anal electromyography (EMG): This test helps determine nerve function and whether or not nerve damage may be causing your rectal prolapse.
- Anal manometry: During this exam, your doctor will insert a small, thin tube into the rectum to test rectal muscle strength.
- Anal ultrasound: An anal ultrasound will help check the muscles and supportive tissues to determine whether they are damage or if there are signs of an internal prolapse.
- Pudendal nerve terminal motor latency test: This test checks to see how well your pudendal nerves function. These nerves control your bowel movements.
- Proctography: A proctography is an x-ray that is performed during a bowel movement to determine how well your sphincter holds and releases feces.
- Colonoscopy: A tiny camera is inserted into your rectum to determine rectal and intestinal health and look for any signs that may be causing a prolapse.
- Proctosigmoidoscopy: Like a colonoscopy, a small tube with a camera attached will check your intestine for signs of injury, inflammation, scarring, or possible tumors.
- MRI: An MRI will check all of the organs located in the abdomen and pelvic region.
Risk Factors
It is more common for women to develop a rectal prolapse than men. However, if you are older and have a history of long term issues with constipation or pelvic floor issues, you may be at a higher risk of developing rectal prolapse.
Long terms bouts with the following may increase your risk for rectal prolapse:
- History of constipation, chronic constipation or diarrhea
- Constant need to strain while pooping
- Lower back injury or disc disease
- Muscle weakness in your anus or pelvic floor
- Genetics or family history of prolapse or weakened pelvic floor
- Chronic obstructive pulmonary disorder (COPD)
- Benign prostatic hypertrophy
- Injuries or complications with ligaments and muscles that keep your rectums attached to the intestinal wall.
- Congenital bowel disorders like Hirschsprung’s disease or neuronal intestinal dysplasia

How to Treat Rectal Prolapse
In most cases, your doctor will recommend surgery. There are various surgical procedures that can help resolve severe rectal prolapse, but they will depend on the patient’s age, severity of the prolapse, and your exam results. This may also be determined by the colon and rectal surgeons’ preference and experience. The most common colon and rectal surgery include: abdominal rectopexy, laparoscopic rectopexy, suture rectopexy, and perineal surgery.
There are other methods of healing rectal prolapse. In our program, Restore Your Core®, we cover a variety of exercises that help you restore and maintain core and pelvic floor health and function. These are typically strength focused exercises that often help resolve many of the issues our clients are facing. Below are just a few examples of techniques, advice, lifestyle changes, and exercises we encourage in our program.
You don’t have to live in
fear, pain or discomfort
Get back the confidence + lifestyle you love

You don’t have to live in
fear, pain or discomfort
Get back the confidence + lifestyle you love
Non-Surgical Rectal Prolapse Treatment
The majority of people with rectal prolapse will find healing through natural remedies and non-surgical, medical measures. These may include core exercises , dietary restrictions, and medications to aid with constipation. Treatment options may include, but are not limited to:
- Pelvic exercises to help strengthen your pelvic floor muscles, entire core system and rectum
- Staying hydrated, drinking plenty of water, and eating a high-fiber diet may help reduce bowel issues
- Treating a chronic cough to aid in reducing pressure and strain on the pelvic floor muscles
- Avoiding heavy lifting or any core exercises that increase intra-abdominal pressure
- Stool softeners to reduce strain during bowel evacuation




