Resources
- Understanding Pelvic Organ Prolapse: What You Need to Know
- Prolapse After Hysterectomy: A Comprehensive Guide to Risks and Prevention
- Can You Have Intercourse With Prolapsed Uterus?
- I Healed My Prolapse: How Targeted Exercises Helped Me
- The Intersection of Prolapse & Weightlifting: What Athletes Should Know
- Hip Mobility and Prolapse: Connection & Exercises to Mitigate Prolapse Symptoms
- Effective Exercises for Relief and Recovery from Prolapsed Uterus
- Uterine Prolapse
- Rectal Prolapse
- How Common is a Prolapse After a Hysterectomy?
- How to Stop a Prolapse from Getting Worse
- Prolapse Surgery
- What is Cystocele?
- Rectocele Repair | Surgery or Exercise
- Rectocele Symptoms : The Signs of Rectocele Dysfunction

FREE video support with Lauren Ohayon
*No spam, just quality
content and support
Resources
- Understanding Pelvic Organ Prolapse: What You Need to Know
- Prolapse After Hysterectomy: A Comprehensive Guide to Risks and Prevention
- Can You Have Intercourse With Prolapsed Uterus?
- I Healed My Prolapse: How Targeted Exercises Helped Me
- The Intersection of Prolapse & Weightlifting: What Athletes Should Know
- Hip Mobility and Prolapse: Connection & Exercises to Mitigate Prolapse Symptoms
- Effective Exercises for Relief and Recovery from Prolapsed Uterus
- Uterine Prolapse
- Rectal Prolapse
- How Common is a Prolapse After a Hysterectomy?
- How to Stop a Prolapse from Getting Worse
- Prolapse Surgery
- What is Cystocele?
- Rectocele Repair | Surgery or Exercise
- Rectocele Symptoms : The Signs of Rectocele Dysfunction
Understanding Prolapse After Childbirth
By Lauren Ohayon 07/04/2024
6 Min Read
Childbirth is the primary risk factor for pelvic organ prolapse. While it is impossible to prolapse-proof your birth process, having a better understanding of prolapse can help you better manage any symptoms and support your postpartum health and well-being.
Table of Contents
How Common is Prolapse After Childbirth?
Approximately one-third to one-half of individuals who have given birth experience some degree of pelvic organ prolapse as a result of childbirth. Although this may seem to be an alarming statistic, the vast majority of these cases are asymptomatic, and many people are unaware of the prolapse. Vaginal births with operative assistance (e.g., forceps, vacuum, etc.) pose the highest risk for POP.
Given that it’s impossible to eliminate the risk of prolapse, I’m going to focus on strategies to reduce the likelihood of needing interventions during birth and ways to recover postpartum that support your pelvic floor health overall.
Understanding Postpartum Prolapse
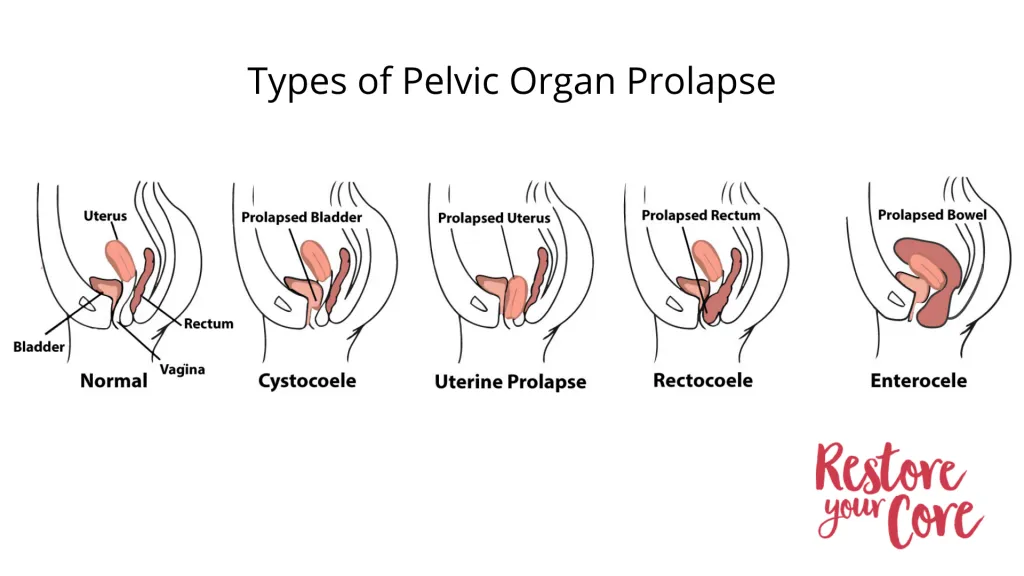
Pelvic organ prolapse is the displacement of one or more pelvic organs into the vagina from their usual positions. There are several types of prolapse:
- Bladder Prolapse- Cystocele
- Rectum Prolapse- Rectocele
- Uterine Prolapse
- Small Intestine Prolapse- Enterocele
- Vaginal Vault Prolapse-only applies to those who have had hysterectomies
The most common prolapses experienced postpartum are bladder, uterine, and rectal prolapses. While it’s not always clear why some people develop prolapse while others in similar circumstances do not, the number of pregnancies, connective tissue disorders, high infant birthweight, high body weight of the birthing person, and other genetic factors are known contributors.
Interestingly, symptoms of pelvic organ prolapse due to childbirth might not show up until much later in life, even 30+ years postpartum. Some speculate that the delay could be due to initial, undetected tearing or damage to the levator ani muscle and changes to tissue strength driven by hormonal shifts during perimenopause.
While the factors that predispose individuals to prolapse vary, most prolapses are exacerbated by excessive intra-abdominal pressure (IAP). This pressure refers to the force exerted within the abdominal cavity. Your body usually manages IAP with the combination of breath, postural alignment, and the coordinated activation and relaxation of the core and pelvic floor muscles. Everyday activities can increase intra-abdominal pressure, including sneezing, coughing, and laughing, and engaging in high-impact exercises such as running and jumping. Additionally, during pregnancy, the growing fetus adds significant pressure on the pelvic floor, which is further intensified during childbirth as the baby moves through the birth canal.
So it’s no wonder that instrument-assisted vaginal deliveries have a much higher incidence of prolapse. Anything that you do that increases the pressure on the pelvic floor during delivery will increase the risk of prolapse. This includes extended pushing phases, precipitous deliveries, prolonged labor, delivery of multiples, high birth weight babies, etc. A tight pelvic floor that is unable to yield to the pressure of birth is another factor.
Signs and symptoms of postpartum prolapse
- How do you know that you have a prolapse postpartum?
- A feeling of heaviness or dragging in the pelvis or and/or genitals
- “Stuck tampon” feeling, like there’s something stuck in your vagina
- Bulge or lump you can feel or see in or just outside your vagina
- Pain or lack of sensation during intercourse
- Urinary issues: bladder not emptying completely, leaking when you sneeze, etc.
- Sometimes, pelvic organ prolapse has no symptoms and is discovered during a pelvic exam
If you’re experiencing any of the symptoms on the list, first off, be patient. Unless your symptoms are severely debilitating, give your body a few weeks to recalibrate after the disruption of pregnancy and childbirth. Like with other pelvic floor and core issues that can result from pregnancy and childbirth, many of your symptoms may resolve in the first few weeks and months postpartum. However, everyone benefits from focusing on pelvic health before, during, and after pregnancy.
How to Avoid Prolapse After Childbirth? Preventive Measures
There are many effective ways to strengthen and prepare your body for pregnancy and birth that may help reduce the risk of developing prolapse. Even if prolapse does occur, your symptoms and severity of prolapse may be reduced.
Stress matters; the musculature of the pelvic floor is greatly affected by our ability to manage stress. A well-supported, low-stress pregnancy will better enable your pelvic floor to yield and manage intra-abdominal pressure during pregnancy and delivery. A birth team that helps support you and encourages multiple ways of moving through your labor and delivery can be key to having a better childbirth experience.
I like to think of prehab and rehab as two phases that are equally important when it comes to pelvic health.
Prehab
Before and during pregnancy, a varied movement menu that includes specific exercises to improve the function of your pelvic floor and core is essential. Of course, the usual advice about nutrition and hydration applies here, too, but you’ll hear plenty of that from your healthcare providers. While prenatal yoga is often touted as great exercise during pregnancy, you should also incorporate plenty of walking, even if that walking slows down quite a bit toward the end of your pregnancy.
Any prenatal exercise plan you embark on should meet you where you are in terms of fitness and should include exercises that help to relax your pelvic floor muscles. Already doing a bunch of strength training? Great! Adjust the kinds of exercises you do to accommodate your changing body and incorporate additional mobility training–not just stretching, but controlling the movement through your range of motion. If you’re particularly athletic and have the resources to do so, a consultation with a pelvic health PT during pregnancy can be invaluable. The PT can help develop a tailored exercise plan that supports pelvic health throughout your pregnancy.
What you want to avoid: adding excessive increased pressure to the pelvic floor. That doesn’t mean that you have to stop running if you’re already a runner! It just means that you need to pay attention to how your body responds to your exercises. How do you know you need to re-evaluate an exercise: are you holding your breath? Sucking in your belly or clenching your abs? Bearing down? Pushing your belly out? (Not sure what those look like? This video may help.) All of these core engagement strategies will increase intra-abdominal pressure.
There are plenty of great exercises to consider before and during your pregnancy. Pregnancy-specific exercises that help to strengthen, lengthen and improve your muscle control and active range of motion will help support your recovery. You also want to be mindful of practices that focus on relaxing the pelvic floor; having a pelvic floor that can yield during labor will reduce the risk of complications. This sequence is full of delicious movements for your pregnant body. Be sure to modify these to suit what feels good to your body.
Rehab
Postpartum rehab is complicated for several reasons: you’re adjusting to a new baby, including feeding that baby, irregular sleep schedules, and the very normal process of your internal organs reorganizing themselves. However, you can begin very gently by introducing movements that help wake up your core and pelvic floor muscles, along with exercises you can do even while seated. Finding a few minutes each day to allow yourself to exist outside of the parent role is essential, even five minutes lying on the floor and letting yourself breathe can be deeply restorative.
It’s out of my scope to offer nutritional advice, but one thing I will tell you is to focus on foods that nourish you on all levels. Please don’t limit your food intake so that your body can get smaller. The goal is to support your healing and your ability to be present and focused on your child.
That said, you can begin walking as soon as you’re comfortable being upright for more than a few minutes. Getting yourself and your baby outside and moving is great for your mental health, too. If you’re noticing a lot of discomfort, take things slowly and gradually at first–especially if you had a C-section or episiotomy. Make sure not to put too much pressure on your incisions.
Early Postpartum Exercises
The following exercises can be helpful for reconnecting with your body as you recover from birth and begin learning how your postpartum body feels.
Arm Rotations can be performed standing or seated
- Stretch one arm out to the side with your palm facing up, as if holding a bowl of water
- Rotate from the shoulder (not the wrist) as if you’re spilling water behind you
- Then rotate in the opposite direction
- For both directions, focus on keeping the movement in the shoulder and arms, not the chest or back
- Explore a variety of angles for a total of 5-8 repetitions, then repeat on the other side

Pelvic Tilts help to reduce tension and restore balance to the pelvic floor muscles
- Lie on your back with your feet flat and your knees bent
- Bolster your head with a folded-up towel or blanket for added comfort
- Begin to tuck and untuck your pelvis gently, as if you’re bringing your pubic bone towards your nose and then away from your nose
- Keep tilting your pelvis forward and back until you feel it moving easily
- Optional: add in some side-to-side tilts:
- Come back to a neutral pelvis
- Imagine that you’ve got a clock on your pelvis, with 12:00 and 6:00 at your navel and your pubic bone
- Tilt your pelvis side to side, from 9:00 to 3:00
- Come back to neutral and tuck and untuck again a few times
- Let your movements be gentle and easy
Floor Angels are fantastic for counteracting the hunched-over posture that many develop while caring for infants.
- Bolster your upper body so that you can recline comfortably, or use the position described below for the psoas release
- Stretch your arms out to the sides away from your body, with your palms facing up
- Slowly sweep your arms along the floor, letting your arms rise away from the floor, rather than arching your back
- Allow yourself to explore as many angles as you like here, then rest your arms and notice how your whole body feels

Psoas Release helps your nervous system reset.
- Lie on the floor with your head and shoulders on a bolster or stack of folded towels, making sure nothing is underneath your lower ribs
- Place a block or towel under your head so that the back of your neck is long
- Prop yourself up high enough that the backs of your thighs are touching the floor
- Relax in this position for 5-10 minutes
Psoas Release on a Block is a variation that can feel particularly good if you do have prolapse symptoms.
- Lie on your back with knees bent and feet planted on the floor
- Prop your pelvis up on a block or bolster (or a pile of pillows or blankets–about 5-6 inches is a good height to aim for
- Allow your whole body to relax here for 5-10 minutes
- Slowly slide the support out and allow yourself to rest on the floor for a few moments to notice how your body feels
How to fix prolapse after childbirth?
You did your prehab and your rehab, but you’re still having symptoms. What’s next? Check in with your OB/GYN.
Once your prolapse is diagnosed, you will most likely be referred to a pelvic health physical therapist. You’ll be given exercises to complete both in office and at home. You may also be fitted with a pessary–kind of like a crutch but for your vaginal walls. A pessary helps provide the support that the tissues of your pelvic floor are no longer capable of providing. There are plenty of exercises you can do at home to supplement your medical team’s advice: my program Restore Your Core® provides a comprehensive, progressive approach to healing pelvic floor conditions.
If your prolapse remains bothersome a year after childbirth and does not improve with physical therapy or pessary use, you might be referred to a surgeon to discuss repair options. There are several surgical approaches for prolapse repair. Make sure you seek a second opinion and do research on the repair that is recommended. Recovering from abdominal surgery can be extensive, requiring significant rest and continued physical therapy.
Managing Prolapse Long Term
Pelvic organ prolapse can be successfully managed long-term, with a significant reduction in symptoms. Many women who experience pelvic organ prolapse as a result of childbirth find that they’re able to go about their daily lives with a fair amount of comfort and ease as long as they’ve been maintaining their pelvic floor health with targeted exercises. Some lifestyle adjustments, such as attention to the way that you’re sitting, standing, and performing activities, can also be helpful, and therapy can help you cope with the changes in your body.
I encourage you not to give up on your body or think that it’s broken. Don’t hesitate to seek help. So often, I see parents who are exhausted from caregiving and who are in pain and discomfort from birth injuries that happened years ago. You deserve to feel at home in your body, too. When you take care of yourself, you can better care of everyone else.
FAQ
1. What exactly is prolapse, and why does it occur after childbirth?
Prolapse refers to the descent of pelvic organs (such as the bladder, uterus, or rectum) into or outside the vaginal canal. This condition occurs when the pelvic floor muscles and ligaments, which support these organs, become weakened or stretched. Childbirth is a common cause of prolapse due to the physical strain and stretching of these supporting structures during labor and delivery. Factors such as prolonged labor, large baby size, use of forceps, and multiple deliveries can increase the risk of developing prolapse.
2. How common is prolapse among postpartum women?
Prolapse is relatively common among postpartum women, with estimates suggesting that up to 50% of women experience some degree of pelvic organ prolapse following childbirth. However, the severity can vary widely, with many cases being mild and asymptomatic. Only about 10-20% of postpartum women experience symptoms severe enough to require medical intervention.
3. How is prolapse diagnosed after childbirth?
Diagnosis of prolapse typically involves a pelvic exam conducted by a healthcare provider. During the exam, the provider may ask you to bear down as if having a bowel movement to better see any descent of the pelvic organs. Additional tests, such as ultrasound or MRI, may be used in some cases to assess the extent of prolapse. The diagnosis often involves grading the prolapse on a scale from 1 (mild) to 4 (severe) based on how far the organs have descended.
4. What are the first steps to take if you suspect you have prolapse after giving birth?
Consult a healthcare provider first: Seek medical advice to confirm the diagnosis and discuss treatment options. Reduce how much intra-abdominal pressure you have to manage by avoiding heavy lifting, running, jumping, etc. Treatment options may include pelvic PT and exercises, pessaries, or surgery.
5. How effective are pelvic floor exercises in treating prolapse?
Pelvic floor exercises are often very effective in treating mild to moderate prolapse. Regularly performing these exercises can strengthen the pelvic floor muscles, reduce symptoms, and prevent the condition from worsening. Many women experience significant improvement in their symptoms with consistent practice.
6. How can prolapse affect long-term health and quality of life?
Prolapse can have various impacts on long-term health and quality of life, including:
- Physical discomfort: Symptoms like a feeling of heaviness or pressure in the pelvic area, urinary incontinence, and difficulties with bowel movements.
- Sexual dysfunction: Pain or discomfort during intercourse can affect intimate relationships.
- Emotional and psychological impact: The physical symptoms and limitations can lead to stress, anxiety, and decreased self-esteem.
- Activity limitations: Prolapse can restrict the ability to engage in physical activities, affecting overall fitness and well-being.



