Uterine Prolapse
4 Min Read
A uterine prolapse occurs when the pelvic floor becomes weakened and the surrounding tissues, muscles, and ligaments are unable to provide proper support to the uterus. This may lead to the uterus descending down or into the vagina. In more severe cases, the uterus may protrude out of the vaginal opening.
Although uncommon, some complications may arise if left untreated. An ulceration of exposed tissues or additional prolapses may occur: rectal or bladder.
However, there are many different treatment options available to you! In this article we address uterine prolapse and how you may find treatment without the need of surgery.
Table of Contents
What is a Prolapse?
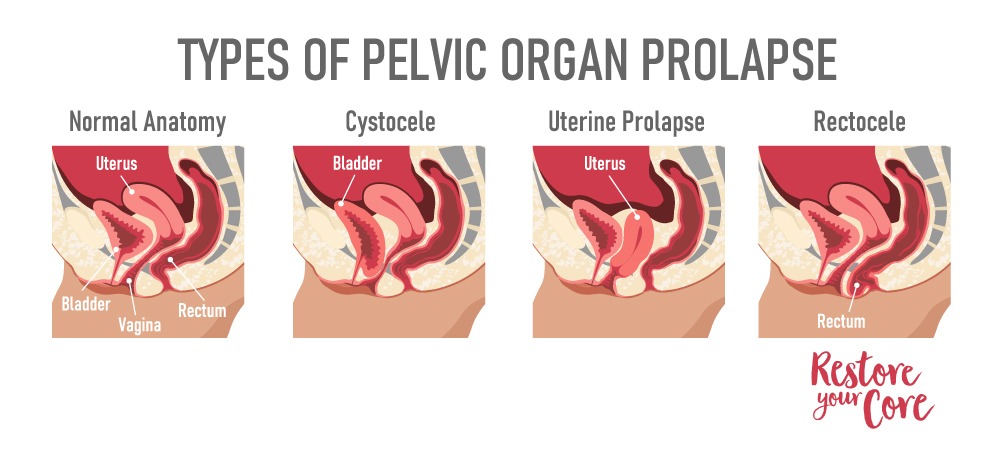
A prolapse or a pelvic organ prolapse, happens when 1 or more organs become displaced. They can either bulge into the vaginal canal or into the rectum. The most common forms of prolapse are uterine prolapse, bowel (rectal) prolapse, and bladder prolapse.

Are you looking for safe and restorative exercises to heal your pelvic floor symptoms?
Learn more about the RYC program.
Are you looking for safe and restorative exercises to heal your pelvic floor symptoms?
Learn more about the RYC program.
These conditions are not life threatening, but may cause painful or uncomfortable symptoms.
In many cases, we at RYC®, have noticed that these symptoms are often relieved and treated through corrective exercise and various lifestyle changes.
What is a Prolapsed Uterus?
Uterine prolapse is a particular kind of pelvic organ prolapse. Although it is more common during pregnancy and childbirth, a uterine prolapse can occur in women of any age and stage of life. Women who are postmenopausal or have had multiple deliveries may be at a higher risk of developing a uterine prolapse.
However, in many cases, surgical treatment is not required. A mild or minor prolapse may resolve through minor lifestyle, exercise, or diet changes. Some providers recommend surgery when prolapse causes pain or unbearable discomfort that interrupts your daily life.
Stages of Uterine Prolapse
A uterine prolapse is often categorized in two different ways: incomplete or complete.
An incomplete uterine prolapse is defined by a partial displacement of the uterus into the vagina, without protrusion.
A complete uterine prolapse is defined by a partial or full protrusion of the uterus out of the vaginal opening. A complete prolapse is then graded in severity, depending on how far the uterus has descended.
- 1st grade: when the cervix has descended into the upper vagina
- 2nd grade: the cervix has descended to the vaginal opening
- 3rd grade: the cervix has protruded outside of the introitus
- 4th grade: the uterus and cervix have both descended out of the vaginal opening
In many cases, exercise may be able to help. In severe cases there may be a need for medical treatment. If you have concerns, it is always best to consult a health professional for a diagnosis.
Symptoms of a Uterine Prolapse
There are many different symptoms that may arise depending on the severity. The most common symptoms of uterine prolapse include:
- a feeling of heaviness or pulling in the pelvic floor muscles
- increased vaginal discharge or vaginal bleeding
- painful or difficulty having sex
- urinary incontinence or urinary retention, leakage of urine
- chronic constipation, bowel movement difficulty
- lumbar spine pain
- bulge or protrusion from the vaginal opening
- pain or dullness in the ovarian ligament, uterosacral ligaments, or in the broad ligament leading to
- a feeling or sensation of something falling from the vagina or like sitting on a ball
- weak vaginal tissue
- pain during sexual intercourse

In many cases, prolapse may be asymptomatic. However, in the presence of symptoms, they often become worse or more noticeable at the end of the day.
What Causes Uterine Prolapse?
Although the cause of many forms of prolapse is not entirely known, there are some common factors and health conditions that may put you at risk of developing a prolapse.
- pregnancy
- delivery complications
- postmenopause, in conjunction with drastic hormonal changes
- heavy lifting, emproper muscle engagement
- straining during bowel movements
- chronic coughing
- muscular atrophy conditions
- genetic conditions
- past pelvic surgeries or operations
Prolapsed Uterus Treatment
If you search online, you will find a host of different sites telling you you need to do kegels or have surgery in order to properly treat a uterine prolapse. Although that may be an answer for some, it is not always the case. Kegels may encourage improper engagement of the pelvic muscles, especially if they are already hyper toned.
A minor / moderate prolapse may be resolved with:
- treating and preventing chronic constipation (high fiber diet)
- avoiding heavy lifting for a time
- properly engaging different muscle groups when lifting is necessary
- treating a chronic cough
- exercise and diet changes
- during menopause, considering hormonal therapy
If you have attempted to prevent your prolapse from getting worse through exercise and treating symptoms like a cough or constipation, medical treatment may be necessary.
Uterine Prolapse Surgery
In the case of a severe prolapse that does not resolve through exercise or physical therapy, your doctor may recommend prolapse repair surgery. A minimally invasive procedure (laparoscopic surgery) or a more invasive vaginal surgery might be an option.
These surgeries often involve:
- Repair of weakened pelvic floor muscles and tissues: This procedure is intravaginal or intra-abdominal. The surgeon may repair the tissues via graft, donor tissue, or with synthetic material to help support your pelvic organs.
- Removal of your uterus (hysterectomy). In very severe cases, a hysterectomy may be advised. Although generally considered safe, any surgical procedure holds a risk of complications.
Before considering surgery as an option, it is best to consult with your doctor and surgeon to ensure you are aware of any risks and benefits prior to your operation.
How to Heal Prolapse Without Surgery
Posture: Pelvic Alignment and Reducing Abdominal Pressure:
Our posture and how we use our bodies in our daily activities significantly impacts our overall core and pelvic floor health. Our posture can greatly affect our joints, muscles, and bone health. When it comes to working with my clients on their rectocele, I always ensure part of their treatment involves restoring and healing their pelvic floor function. An unintentional mistake many women make when standing upright is shifting their weight forward in their hips. Think of the hips leaning forward. This shift can actually increase tension in the muscles of the pelvic floor leading to varying types of POP. In the process of resolving pelvic alignment, I might work on hamstrings, upper back mobility, glute function, pelvic mobility and more. Resolving pelvic floor issues requires us to view the pelvic floor as a part of an entire system and therefore requires a whole-body approach. The process of learning how to align your body to better support you while you stand takes time, but is well worth the process. And your pelvic floor will thank you for it! Better alignment = less pelvic floor tension and pressure.
Now that you know that rectocele can be treated without the need of surgery, it may be time to learn more about how to use exercise to heal your pelvic floor. My 13 Week Program: Restore Your Core offers a step by step approach to developing a strong, healthy, responsive core & pelvic floor system, for the health of your whole body.
You don’t have to live in
fear, pain or discomfort
Get back the confidence + lifestyle you love

You don’t have to live in
fear, pain or discomfort
Get back the confidence + lifestyle you love
Pelvic Floor Exercises
Tadasana – Mountain pose
A mountain pose is a standing pose which engages your abdomen, pelvic floor, and back.

Stand with your big toes together and your heels slightly apart. Ensure that your weight is distributed evenly between your feet. Relax your arms at your side with palms and biceps facing forward. Inhale, and gently lift your ribcage to be evenly distanced from your pelvis. Place your palms gently on your sides for lower back stability, and exhale slowly. Repeat 5 – 10 times as you are able.
Pelvic bridges
A pelvic tilt is beneficial in strengthening your lower and upper back as well as your hips and legs.

To begin, lie on your back with your feet aligned with your hips and your arms resting at your sides, palms face down. Gently curl your tailbone so that your spine is settled on the floor. This will relieve any pressure you may feel in your lower back. Inhale and begin slowly exhaling as you gently lift your hips upward, tilting your pelvis as you continue tucking in your tailbone. Hold for 2 – 3 breaths and slowly lower yourself back to your starting position. Repeat 5 to 10 times as you are able.
It is important that if you feel any pain or discomfort during these exercises, that you pause and wait until you are able.




