Resources
- Understanding Pelvic Organ Prolapse: What You Need to Know
- Prolapse After Hysterectomy: A Comprehensive Guide to Risks and Prevention
- Can You Have Intercourse With Prolapsed Uterus?
- Understanding Prolapse After Childbirth
- I Healed My Prolapse: How Targeted Exercises Helped Me
- The Intersection of Prolapse & Weightlifting: What Athletes Should Know
- Hip Mobility and Prolapse: Connection & Exercises to Mitigate Prolapse Symptoms
- Effective Exercises for Relief and Recovery from Prolapsed Uterus
- Uterine Prolapse
- Rectal Prolapse
- How Common is a Prolapse After a Hysterectomy?
- How to Stop a Prolapse from Getting Worse
- Prolapse Surgery
- Rectocele Repair | Surgery or Exercise
- Rectocele Symptoms : The Signs of Rectocele Dysfunction

FREE video support with Lauren Ohayon
*No spam, just quality
content and support
Resources
- Understanding Pelvic Organ Prolapse: What You Need to Know
- Prolapse After Hysterectomy: A Comprehensive Guide to Risks and Prevention
- Can You Have Intercourse With Prolapsed Uterus?
- Understanding Prolapse After Childbirth
- I Healed My Prolapse: How Targeted Exercises Helped Me
- The Intersection of Prolapse & Weightlifting: What Athletes Should Know
- Hip Mobility and Prolapse: Connection & Exercises to Mitigate Prolapse Symptoms
- Effective Exercises for Relief and Recovery from Prolapsed Uterus
- Uterine Prolapse
- Rectal Prolapse
- How Common is a Prolapse After a Hysterectomy?
- How to Stop a Prolapse from Getting Worse
- Prolapse Surgery
- Rectocele Repair | Surgery or Exercise
- Rectocele Symptoms : The Signs of Rectocele Dysfunction
What is Cystocele?
By Lauren Ohayon 09/26/2020
4 Min Read
Cystocele is the most common type of pelvic organ prolapse that occurs after vaginal childbirth. During a vaginal delivery, the pelvic floor muscles can be compromised as they stretch to make room for the baby to make its grand entrance into the world. The pelvic floor muscles are designed to hold up the organs of the pelvis. A severe enough breach in the system can cause a prolapse.
When these muscles are compromised, the organs are able to drift or “sag” down the path of least resistance until they bulge into the vaginal canal. It is important to know that there are many types of pelvic organ prolapse besides cystocele that will not be discussed in this article, but are listed below for educational purposes:
-
- Urethrocele or prolapse of the urethra
-
- Uterine prolapse
-
- Vaginal vault prolapse
-
- Enterocele or prolapse of the small bowel
-
- Rectocele prolapse of the rectum
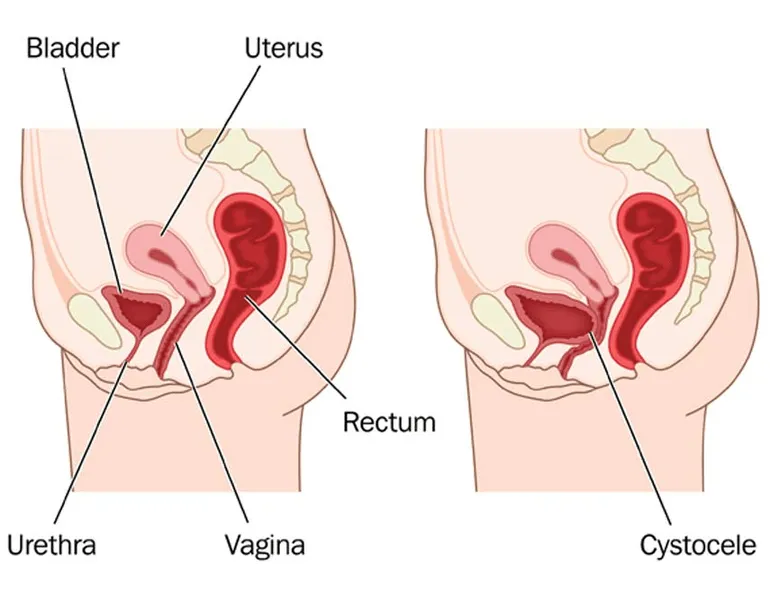
Table of Contents
What causes a Cystocele?
Cystocele (cysto- meaning bladder, -cele meaning pouching or herniating) is the downward displacement of the bladder that descends until the bladder bulges into the vaginal wall. This is sometimes referred to as “fallen bladder” or “prolapse of the bladder.” Though it is possible that cystocele occurs because of reasons outside of childbirth, such as genetic disposition, increased age or obesity, it is most commonly seen in women who have experienced a vaginal delivery.
How is a cystocele diagnosed?
Methods of diagnosis depend on how much the prolapsed bladder has advanced from its usual position.
The pelvic exam is used for the obvious prolapsed bladder. The provider may only need to do a visual exam of both the vaginal opening and the pelvis to spot the bladder in late staged prolapse (I’ll break down the stages for you momentarily). Typically this presents as a pronounced bulge in the vaginal canal or through the opening of the vagina. I strongly recommend doing this exam from a standing position.
A voiding cystourethrogram may be used in less obvious cystoceles since the prolapsed bladder is not always visible In the vaginal opening in earlier stages of descent. Essentially, an X-ray is taken of the bladder while you urinate to capture the shape and placement of the bladder and vagina during the effort. Your provider will guide you through the preparation for this procedure, but there are typically no special precautions needed.
What are the symptoms of Cystocele?
Symptoms of a cystocele vary from mild, moderate or severe depending on just how far that bladder has sagged from its usual position.
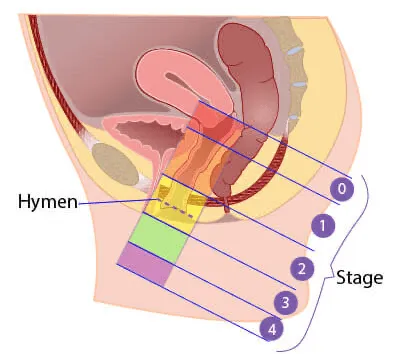
The Grading System
-
- Grade 1 Cystocele: is mild, and is when the bladder drops only a short way into the vagina or if we are being technical, >1 cm above the hymen. Mild cystocele symptoms may include stress urinary incontinence, which is a fancy way of saying the laugh pee, cough pee, sneeze pee, or during times of sudden exertion (run pee). Other symptoms include urinary frequency and nighttime voiding (the night pees). If the bladder is also unable to empty completely upon urination, it is not uncommon to have frequent bladder infections.
-
- Grade 2 Cystocele: is considered moderate, and occurs when the bladder drops far enough to reach the opening of the vagina. If we are being technical, less than or equal to 1 cm from the hymen. Symptoms of moderate cystocele can include all of the previous issues around urine as well as a feeling of “fullness” in your vagina, a dragging sensation in the vagina, sexual dissatisfaction, and you may be able to begin seeing the bladder through the opening of the vagina.
-
- Grade 3 Cystocele: involves partial bladder passage through the opening of the vagina upon exertion and is considered severe.
-
- Grade 4 Cystocele: is the extrusion of the bladder base beyond the vaginal opening at rest to maximum possible descent. Yes, this means your bladder is able to all but exit the body through the vaginal opening. The vagina and bladder are now prolapsed. It is at this stage in which one’s experience may include urinary retention, which if left untreated can lead to kidney damage or infection.
How Can You Tell if you have a Bladder Prolapse?
Typically the first tell tale sign is a feeling of bulging in your vagina, heaviness, fullness, feeling of bubbles in your vagina and a change in your urine frequency/incontinence after a vaginal delivery that doesn’t improve over time.
If it is more advanced you may be able to see the bulge formed by the bladder prolapse in the canal or vaginal opening. Heavy lifting, bearing down or straining during bowel movements may increase the feeling of pressure in the pelvic floor. Some women report feeling as if they are sitting on a ball.
What do I do if I Suspect Cystocele?
If you experience any of these, contact your health care provider for further investigation to get you on the best track to getting back a healthy pelvic floor. Restore Your Core® has a Cystocele-specific workout program that we recommend to our community of ladies (if you’d like to join the community, you can find our group of 20K+ women here). It is important to note that we always recommend talking with a doctor to get an official diagnosis.
How do you treat Cystocele?
We always recommend conservative treatment as a first step. The typical goal of conservative treatment is to improve symptoms, reduce progression, and all together avoid or delay surgical treatment. Providers may talk to you about hormone therapy and other cystocele treatments that fit your unique medical picture.
Please note: Typically at the beginning of treatment, heavy lifting or straining during bowel movements should be avoided.

How Long is Recovery from Bladder Prolapse?
For some women, cystocele repair may include an inevitable surgical option. Although it is not always necessary, there are times when some women may experience the care and relief they need surgically. We at Restore Your Core® are not your physician, but seek to offer the most insight we can to provide the best options available for symptom control and your general well-being.
If you do happen to seek surgery for your bladder prolapse, you may be in recovery for 6 weeks to longer depending on the extent of the surgery performed and the severity of your prolapse. During these 6 to 8 weeks, you should avoid any strenuous activities: heavy lifting (don’t lift anything heavier than a gallon of milk), or standing for long periods of time for at least the first 3 months. Avoiding any activities that may place too much pressure on your bladder or lower abdomen will be crucial to your recovery. After the first 6 weeks, try reintroducing light exercise and begin regaining your strength gradually.
How can we help you along your cystocele journey?
I have spent 20 years developing a method that addresses core and pelvic floor dysfunction from a functional perspective. What that means is that we address the compromise, the injury from a very “whole body” perspective. We see the pelvic floor as a system that is connected, dependant upon other systems. Pelvic positioning, posture, breathing, spine mechanics, all affect the pelvic floor. Our approach is not a spot treatment one. We do not simply say “do your kegels.” That is a pretty old school method that often does not work and can make things worse. Rather, we look at the whole of you and help you determine what your movement compensations are so you can help your pelvic floor become reflexive, responsive and supportive to your organs and body once again.
Cystocele Recovery with Restore Your Core®
It is important to understand that our overall health can be significantly impacted by the way in which we move. My 12 Week Program: Restore Your Core® offers a step by step approach to developing a strong, healthy, responsive core & pelvic floor system, for the health of your whole body. Restore Your Core® seeks to train women to intelligently and holistically heal from core and pelvic floor disorders while educating them on how their body’s function and how to properly engage their bodies during their daily activities.
To learn more about the various exercises that assist in core strength and resolving core and pelvic floor pain, check out one of my previous blog posts.



