How to Stop a Prolapse from Getting Worse
4 Min Read
You did it. You birthed a bouncing baby and your body is in recovery from enduring the sheer awesomeness that is childbirth. As the months that follow unfold and that baby starts to grow, you can’t help but shake the feeling that something is not quite right down there. Why is peeing so weird now? When did my body decide it was okay to just leak out said pee every time I cough? Am I supposed to just wear panty liners all day every day just in case someone makes me laugh? Why does it feel like there is a bulge in my vagina?
Though it is a common post-birth issue, the first time you hear that you have pelvic organ prolapse may be frustrating and quite upsetting. I mean, your body was made to have babies. Why would something so natural cause such an issue?
Table of Contents
Avoiding the S Word
Your doctor may suggest many treatment options to help prevent your prolapse from advancing to the point where they begin to start talking about surgery. Surgery is a SCARY word that we would like to help you avoid. Prolapse reconstruction surgery, or Vaginoplasty, may be recommended in advanced cases. However, if you aren’t severely prolapsed, there are steps you can take that may help you avoid surgery all together. Yes, early prolapse can be corrected without ever ending up under the knife. Even a grade 3.
Popular less invasive treatment offered can include vaginal pessaries and Kegels as the only form of pelvic floor treatment. Don’t hear me wrong, these can be very helpful, but I am more a fan of using a functional, whole body exercise approach to healing core and pelvic floor issues. Here at Restore your Core®, we are fellow partners of your health-focused team and are seriously invested in empowering you to make every movement throughout your everyday life healing. We believe and have seen first hand with many clients, that our 12-week program can train you to bring symptom relief and avoid the discussion of surgery altogether. No matter when you discover a prolapse, we always recommend 1 year of pelvic floor rehab before deciding on more drastic routes.
Pelvic Organ Prolapse: What is it?
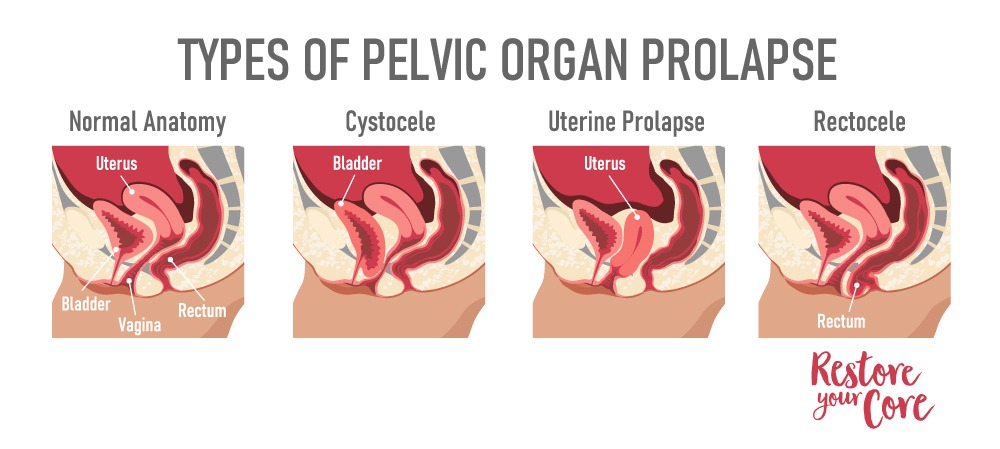
First things first, let’s make sure we are all speaking the same language here: pelvic organ prolapse is the injury in which one or more of your pelvic organs “drop” from their normal position. Though bladder prolapse is the most common, any pelvic organ (bladder, uterus, rectum) can make the descent. This injury happens for a variety of reasons and sometimes, it is really not known why. Birth injury, core and pelvic floor muscle imbalances, postural misalignments, and excess intra ab pressure are all reasons one might sustain a prolapse.
If pelvic organ prolapse is allowed to advance to its fullest potential, the prolapsed organ will make its way down the path of least resistance into the vaginal canal. Eventually, the organ may exit the vaginal opening.
Different types of Pelvic Organ Prolapse include:
- Bladder prolapse- Cystocele (the most common)
- Rectum prolapse- Rectocele
- Uterine Prolapse
- Vaginal Vault Prolapse
- Small Intestine Prolapse- Enterocele
Though pelvic organ prolapse can be caused by obesity, aging, and other stressors on the floor muscles, vaginal birth is the leading cause of prolapse. As you can imagine, vaginal birth does a number on those pelvic floor muscles because of the amount of stretch the pelvic floor muscle must undergo to make way for the baby’s grand entrance into the world. This is why it is pretty common to pelvic floor prolapse after childbirth.
How Do I Know if My Prolapse is Severe?
The severity of Pelvic Organ Prolapse has to be diagnosed by your healthcare provider, but the general rule of thumb for staging is:
- Stage 1: Very minimal prolapse – organs still have a fair amount of support by the pelvic floor.
- Stage 2: Pelvic floor organs have begun to drop, but they are still contained inside the vagina.
- Stage 3: Pelvic floor organs have dropped to, or beyond the opening of the vagina.
- Stage 4: Pelvic floor organs have dropped completely through the vaginal opening.
Stage 3 and 4 are when you may be experiencing the more severe effects of prolapse. If your prolapse is severe, you may experience a wide range of symptoms. Check out our other articles that break down the specifics for different types of pelvic organ prolapse. Some of the most common symptoms for severe prolapse can include but are not limited to :
- the sensation that you are sitting on a ball
- A dragging sensation or heaviness in the vagina
- vaginal bleeding
- increase or change in discharge
- problems with or inability to engage in sexual intercourse
- any pelvic organ protruding out of the vagina
- a heavy feeling in the pelvic area
- The feeling of trapped bubbles in your vagina
- constipation or difficulty passing stool
- recurring bladder infections or difficulty emptying your bladder
- Incontinence, which is the inability to control when you pee.

If you experience any of these, contact your doctor. We recommend seeing a Urogyn to get tested, and ideal is to be tested standing up, not lying down.
What Happens if Prolapse is Left Untreated?
We have many clients who are not symptom free! Unfortunately, if left to its own devices, organ prolapse may continue getting worse if no intervention or treatment measures are taken. Our muscles and skeletal systems are the protectors and stabilizers of our organs. When our pelvic floor is just as strong as the rest of our core, straining and bearing down is countered within the core to keep all the organs in their assigned spots. Once the pelvic floor muscles have been compromised / weakened, they are no longer able to counter the force of your rest of your core.
If your prolapse is the result of a vaginal birth you had, you are likely to be doing some heavy lifting in the day to day life just to take care of your newest addition to your family. Every time you do heavy lifting, the force that is placed on your already prolapsed organ may push it further down the path of least resistance and right into your vaginal tissues. Because of this it is important to begin building a strong organ support system to help prevent pelvic organ prolapse from becoming worse.
Can I push a Prolapse back up?
When our insides decide to try to escape to the outside, it is time to get a professional involved. Though it may actually be possible to temporarily push fully prolapsed pelvic organs back into the vaginal opening, this is not a long term solution or an actual treatment. It is important to seek medical advice and see a pelvic floor therapist if severe symptomatic stage 3 or stage 4 prolapse occurs.
Why is My Prolapse Worse Some Days?
There are times during your cycle where you might feel worse. Hormonal changes can affect how your prolapse feels. This is common and even if you are doing great in your rehab process and this happens, do not panic! Many women feel it worse during ovulation. If you have just finished moving furniture around the house or gotten home from an intense workout just to be greeted with worse prolapse symptoms for the rest of the day, this is actually very normal for many women who suffer with pelvic organ prolapse. Straining on the toilet while trying to work through some constipation can also worsen your symptoms. When doing strenuous activities, we bear down and increase the pressure within ourselves and this can place even more pressure and force on the organs.
What should you not do with a prolapse?
You may have noticed a bulge in your vaginal wall, a lower hanging uterus or experienced a change in your urine, stool, or discharge pattern that makes you suspect a pelvic organ prolapse. As you seek medical advice, it is important to begin to treat your conditions by cutting back on strenuous exercise until you can build up your pelvic floor muscles through direct treatment. Prolapse can be frustrating to deal with to say the very least, but if there must be a silver lining, it is that the doctor has ordered you to get another family member to move that couch.
Here are the things to avoid when you have pelvic organ prolapse:
- Avoid straining while on the toilet
- Avoid being on your feet for long periods of time
- Avoid lifting, pulling or straining
- Avoid an intense workout routine – until you have a great core / pelvic floor strategy.
Here are the things TO DO when you have pelvic organ prolapse:
- Make sure you hydrate frequently throughout the day
- Eat all the fiber. Beans, veggies, fruits, you name it.
- Educate yourself on prolapse, the core system, all of the connections that can increase and decrease pressure.
- Consider a pelvic floor therapist, pelvic floor trained teacher, or Online program to guide you through healing.
How Can I Reverse Prolapse Without Surgery?
Pelvic organ prolapse may be reversed without invasive procedures like surgery. Working on your pelvic floor system in a functional way can begin to reverse the prolapse descent.
If I have not said it enough, I will say it again: always talk to your provider if you are experiencing symptoms that interfere with your daily routine and you are worried about.
Your doctor may recommend Kegel exercises as the only form of pelvic floor muscle treatment. Kegel exercises are the favorite prescription within the medical field for weakness in pelvic floor muscles but it is essentially an old school approach that fails to work for many and makes things worse for many others. We strongly believe in a more functional approach to the pelvic floor – one that incorporates the whole body for healing and works on integrating your pelvic floor into the whole system of pressure, load and movement.

Restore Your Core program was created to offer ways of treatment for women that does not involve just sitting and clenching your pelvic muscles a thousand times over, but rather teaches you patterns of movements that build a functional, responsive core and pelvic floor. RYC® is a whole body approach that takes your daily movements and patterns into account so that you can retrain your body all day long and not just when you are sprawled out on the floor doing your next set of Kegels. To our excitement, our hypothesis was confirmed when we began to hear feedback from women who had restored their core and minimized or eliminated prolapse symptoms. Give us 12 weeks, and we will show you how to champion your own core.




