Prolapse Surgery
4 Min Read
Surgery for pelvic organ prolapse is a big deal. It is a big deal because you live in an age where you have many pathways to health, and don’t have to live with pelvic organ prolapse.Although surgery can be a viable, medically recommended option for many people, it is very invasive without a guaranteed outcome. Some people may find relief from their painful symptoms, yet, like many procedures, it can often require more intensive medical treatmenteven after the first surgery was performed. Surgery should be considered a last option when dealing with core, pelvic floor, or other related issues.
To be clear, our goal here at Restore Your Core is to strengthen your core and pelvic floor so you can live without surgery being a part of your story. Thousands of women use our program with amazing success as an alternative route to surgery because we work to restore function and integrity to the pelvic floor. However, we do not judge anyone’s choice to have surgery and we understand that sometimes it is the only choice! We support all choices so we would like to use this article to educate you on those choices. Please note, even if you decide on surgery, one year of pelvic floor rehab is very much recommended to prepare the body as it is a major surgery.
Table of Contents
How Do I Know if My prolapse is Severe?
Surgery is for severe cases. So when are you considered severe? We strongly urge you to discuss it with your provider and get multiple opinions from doctors and therapists regarding your case.
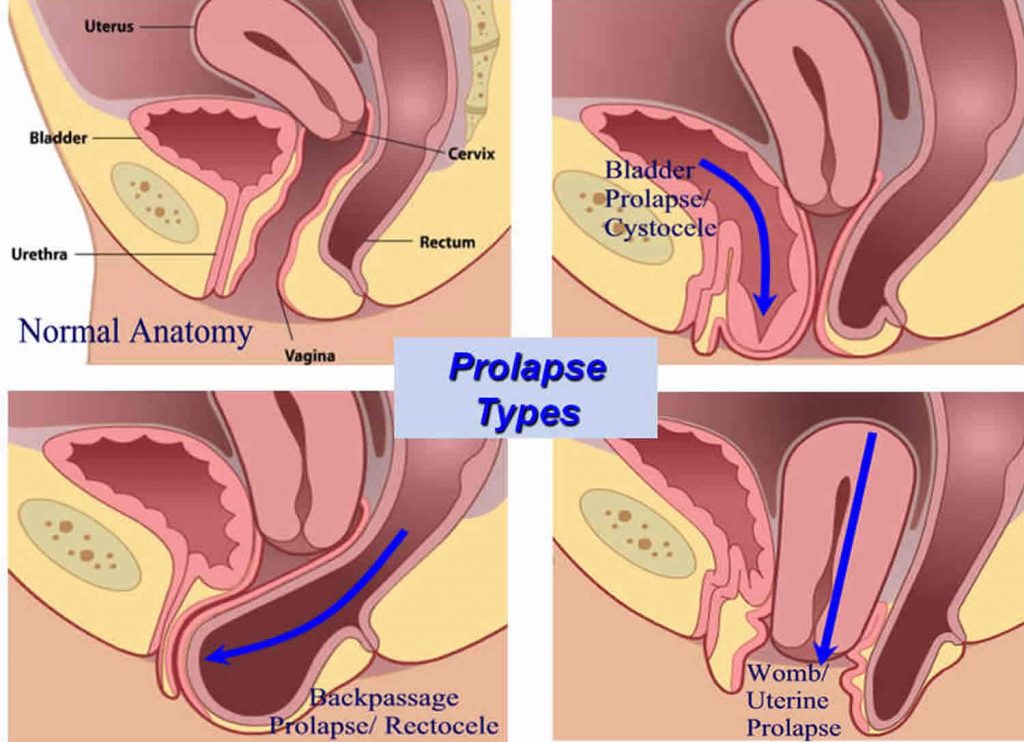
It is important to recognize that pelvic organ prolapse can involve one or more of your pelvic organs, including your uterus, bladder, and rectum. After injury to or the weakening of your pelvic floor muscles, your organs can drop into the wall of your vagina. We break down the different types of pelvic organ prolapse in other articles, but for your knowledge, we will include a list here:
- Bladder prolapse- Cystocele (The most common)
- Rectum prolapse- Rectocele
- Uterine Prolapse
- Vaginal Vault Prolapse
- Small Intestine Prolapse- Enterocele
How Do I Know What Stage My Pelvic Organ Prolapse Is?
Severity of Pelvic Organ Prolapse has to be diagnosed by your healthcare provider, but the general rule of thumb for staging is:
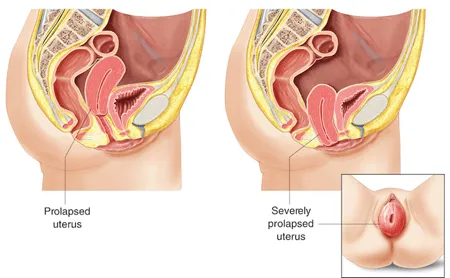
- Stage 1: Very minimal prolapse – organs still have a fair amount of support by the pelvic floor.
- Stage 2: Pelvic floor organs have begun to drop, but they are still contained inside the vagina.
- Stage 3: Pelvic floor organs have dropped to, or beyond the opening of the vagina.
- Stage 4: Pelvic floor organs have dropped completely through the vaginal opening.
What Happens if Prolapse is Left Untreated?
That is hard to know because some women have it for years and it can stay the same! However, for others, it can actually get worse. It can depend on a variety of factors, many might be out of your control: like tissue integrity and genes. Other elements, like movement and exercise choices are more in your control. Strengthening your pelvic floor can keep your organs from bulging further into the wall of the vagina without surgery.
What are the Symptoms of Severe Pelvic Organ Prolapse?
A range of symptoms can be present in any stage of your journey with prolapsed pelvic organs. It is when your symptoms are interfering with your everyday routine or when interfering with other bodily functions that your doctor may talk seriously about surgery for your pelvic organs. Surgery is especially needed when we have organs exiting the body, a vaginal vault starts folding in on itself or your body becomes unable to rid itself of waste. Other symptoms can include:
- the sensation that you are sitting on a ball
- a dragging sensation or heaviness in the vagina
- vaginal bleeding (uterus prolapse)
- increase or change in discharge from vagina
- problems with or inability to engage in sex
- any pelvic organs protruding out of the vagina
- a heavy feeling in the pelvic area
- constipation or difficulty passing stool
- recurring bladder infections or difficulty emptying your bladder
- urinary incontinence, (the inability to control when you pee)
People can often experience a prolapse post birth. Other common causes can be obesity, aging, or other surgery in the pelvic area. It can also be genetic and related to tissue integrity.
Why is My Prolapse Worse Some Days?
There are times during your cycle where you might feel worse. Hormonal changes can affect how your prolapse feels. This is common and even if you are doing great in your rehab process and this happens, do not panic! Many women feel it worse during ovulation. If you have just finished moving furniture around the house or gotten home from an intense workout just to be greeted with worse prolapse symptoms for the rest of the day, this is actually very normal for many women who suffer with pelvic organ prolapse. Straining on the toilet while trying to work through some constipation can also worsen your symptoms. When doing strenuous activities, we bear down and increase the pressure within ourselves and this can place even more pressure and force on the organs.
How Do You Fix a Prolapse?
Many forms and stages of prolapse, or pelvic organ prolapse can be treated by exercises that strengthen the pelvic floor.
However some women need a little extra help getting their pelvic organs to stay where they are supposed to be. In these cases, surgery may become a necessary part of the journey. When it comes to surgical prolapse repair, there is no one size fits all reconstructive surgical option. Since we are not doctors, we do not give medical advice. The following is simply educational material and not intended as a form of medical advice. The type of surgery for your prolapse depends on your type of prolapse. We set out to tackle some of the most common questions regarding this.
What Types of Surgery are There?
Reconstructive surgery returns organs to their original position while repairing the pelvic floor. This can be done through an incision either in the abdomen or the wall of the vagina. Laparoscopic surgery is also an option here, which just means the surgeon makes smaller cuts in the abdomen while using instruments specialized for the surgery.
Obliterative surgery is the last effort to prevent vault prolapse. This type of surgery is used if other invasive surgeries haven’t worked or can not be tolerated due to other health conditions. During this procedure, the vagina is narrowed or all together closed up. The goal is to provide more support to the organs that have dropped out of their normal positions and are pressing against the walls of the vagina. This isn’t the first choice because after the surgery, intercourse would no longer be an option.
Sacrospinous ligament fixation and uterosacral ligament suspension surgery. A vaginal mesh of your own tissue is made to improve the support of the uterus. Mesh is placed under the vaginal skin to support the organs that are attempting to sag. Stitches are used to attach the vaginal vault to a ligament on your pelvis.
Anterior and posterior colporrhaphy surgery. The anterior surgery is used for cystocele that bulges through the vagina with urinary incontinence. Surgery is used to make tissue stronger and tighter. Posterior repair is used when in rectocele that has dropped prominently into the vagina. This procedure often uses mesh as well as existing tissue to repair the sagging organs done through the vagina by using your own tissues or vaginal mesh to repair the prolapse.
Sacrocolpopexy and sacrohysteropexy surgery. Both of these procedures focus on anchoring organs with mesh. Sacrocolpopexy is used to repair vaginal vault prolapse. Sacrohysteropexy is used to fix prolapse uterine. These can be done laparoscopically or through incisions on the abdomen.
Can Your Organs Descend After a Hysterectomy?
A prolapse of the uterus is unique because it is the only pelvic organ prolapse in which one of the surgical options is to just remove the problem organ if it will not stay in place. It is said that the traditional approach to uterine prolapse is to remove the uterus through the vagina, otherwise known as a vaginal hysterectomy Other treatment options are vaginal reconstruction, the placement of a pessary. (Of course, there are many other reasons why one would have a hysterectomy.)
The issue with a hysterectomy is it could cause further prolapse of other organs because that sizable uterus isn’t there to claim its space anymore. Also, in doing the hysterectomy the underlying issue that is the weak, stretched out pelvic floor muscles were not dealt with. Information regarding the rate of post-hysterectomy prolapse varies. Currently, cumulative data shows the risk that your pelvic floor does not keep your organs in place is 1% three years after hysterectomy and up to 15% fifteen years later.
This is why it is so important to strengthen your pelvic floor after you have healed from your hysterectomy. Many women who have a prolapsed uterus and want the surgical option will opt for the less invasive laparoscopic surgery or vaginal reconstruction surgery with a vaginal mesh rather than a hysterectomy.
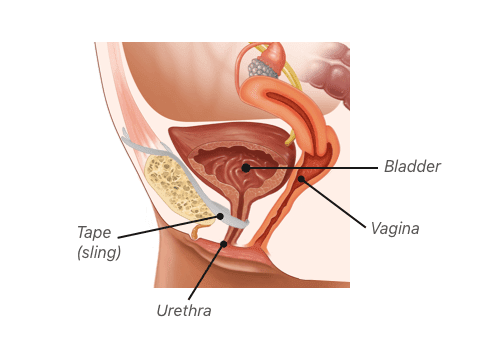
What Type of Surgery is Required for a Prolapsed Bladder?
Cystocele, also known as a bladder prolapse, is one of the most common types of pelvic organ prolapse. The common surgical procedure to attempt to fix this condition is mid-urethral sling surgery. This surgery implants a mesh sling around the urethra, connected to the pubic bone, to help properly re-align the urethra to resolve urinary incontinence (leak pee). However, there are known complications with this surgery. If the mesh sling does not resolve your symptoms, often the surgeon will recommend anterior repair surgery.
Surgery is not something we encourage or discourage our clients to consider. However, if your doctor has recommended surgery as being your best option, it is better to discuss this solution with a medical professional
Is Prolapse Surgery Painful?
As with many surgical procedures, there is a time for recovery that may be painful for some. With pelvic prolapse surgery, your body has undergone a pretty dramatic transition. Post-op, you will most likely be given medication to help reduce pain. Take it as directed by your doctor. It is important that if you are considering, or have received surgery to repair pelvic floor dysfunction that you address any concerns you may have with your healthcare provider.
How Long Does it Take to Recover from Prolapse Surgery?
Your recovery time will be dependent upon the length, type, and invasiveness of your procedure. In some cases, recovery times may only take up to a week or two and in others it may be over a month. When talking with your doctor, be sure to discuss recovery time and what is expected during your recovery.
What Should I Expect After Surgery for Pelvic Organ Prolapse?
We hope that your recovery will be a quick transition back into your daily activities. It is common for many women to experience fatigue, slight bleeding at the surgery site, and to be prescribed pain medication post-op. If you have any concerns or questions regarding the requirements after surgery, it is best to discuss this with your doctor.

As soon as your doctor has confirmed that you have recovered from surgery, we hope that you join us in our 12 week program and learn how to Restore Your Core beyond surgery!




