Resources
- Understanding Pelvic Organ Prolapse: What You Need to Know
- Prolapse After Hysterectomy: A Comprehensive Guide to Risks and Prevention
- Understanding Prolapse After Childbirth
- I Healed My Prolapse: How Targeted Exercises Helped Me
- Hip Mobility and Prolapse: Connection & Exercises to Mitigate Prolapse Symptoms
- The Intersection of Prolapse & Weightlifting: What Athletes Should Know
- Effective Exercises for Relief and Recovery from Prolapsed Uterus
- Uterine Prolapse
- Rectal Prolapse
- How Common is a Prolapse After a Hysterectomy?
- How to Stop a Prolapse from Getting Worse
- Prolapse Surgery
- What is Cystocele?
- Rectocele Repair | Surgery or Exercise
- Rectocele Symptoms : The Signs of Rectocele Dysfunction

FREE video support with Lauren Ohayon
*No spam, just quality
content and support
Resources
- Understanding Pelvic Organ Prolapse: What You Need to Know
- Prolapse After Hysterectomy: A Comprehensive Guide to Risks and Prevention
- Understanding Prolapse After Childbirth
- I Healed My Prolapse: How Targeted Exercises Helped Me
- Hip Mobility and Prolapse: Connection & Exercises to Mitigate Prolapse Symptoms
- The Intersection of Prolapse & Weightlifting: What Athletes Should Know
- Effective Exercises for Relief and Recovery from Prolapsed Uterus
- Uterine Prolapse
- Rectal Prolapse
- How Common is a Prolapse After a Hysterectomy?
- How to Stop a Prolapse from Getting Worse
- Prolapse Surgery
- What is Cystocele?
- Rectocele Repair | Surgery or Exercise
- Rectocele Symptoms : The Signs of Rectocele Dysfunction
Can You Have Intercourse With Prolapsed Uterus?
By Lauren Ohayon 09/05/2024
6 Min Read
One thing that many of my clients with pelvic organ prolapse ask is, “Can you have intercourse with a prolapsed uterus?” The answer is usually yes, but there are some modifications and treatment modalities that can make intercourse much more comfortable and pleasurable.
Table of Contents
Uterine Prolapse and Client Concerns
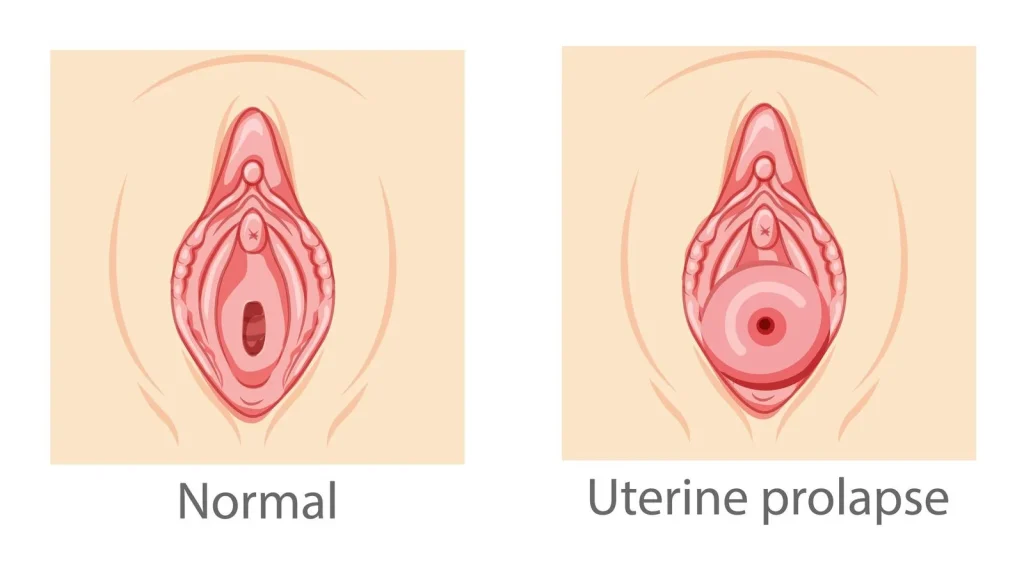
Uterine prolapse is a condition in which the uterus moves out of place, usually due to weakened pelvic floor muscles, ligaments, and other connective tissue. In severe cases, the uterus may protrude out of the vaginal opening. A prolapse is graded in severity, depending on how far the uterus has descended.
Professionals like you who work in the fields of sexual health, gynecology, and pelvic floor therapy are familiar with the symptoms of uterine prolapse. Physical symptoms aside, uterine prolapse can deeply affect a client’s quality of life by making exercise and daily acts of living difficult and uncomfortable. For those patients who are or wish to be sexually active, uterine prolapse may seem like an insurmountable barrier to regular sexual intercourse. Your clients may turn to you for insight into how to maintain an active and satisfying sex life with prolapse.
Overview of Uterine Prolapse
Uterine prolapse is commonly caused by pregnancy and birth, as these events place significant stress on the muscles and connective tissues of the pelvic floor. The risk of prolapse increases with each subsequent pregnancy; however, for those who already have a prolapse, a subsequent pregnancy doesn’t always worsen the condition. The onset of prolapse symptoms can often be significantly delayed, sometimes not appearing until perimenopause or later, well after the initial stress of childbirth. Many people with uterine prolapse may not experience symptoms and frequently go undiagnosed until symptoms eventually manifest.
Common symptoms of uterine prolapse include:
- A sensation of heaviness or pressure in the pelvis
- Feeling or seeing a bulge or protrusion in the vagina
- Difficulty with urination, including urinary incontinence or urinary retention
- Frequent urinary tract infections (UTIs)
- Discomfort or pain during intercourse
- Lower back pain
- Vaginal bleeding or increased vaginal discharge
- Difficulty with bowel movements, including constipation
- A feeling of something “falling out” of the vagina
- Difficulty inserting tampons or them feeling dislodged easily
These symptoms can vary in severity depending on the degree of prolapse. Uterine prolapses are categorized by stages or grades, with an increase in severity that depends on how far the uterus has moved from its usual location. This tool from the American Urogynecologic Society makes visualizing the different types and stages of prolapse easy.
While the stage numbers are useful, the focus of most patient treatment and counseling should be on patient needs and concerns. Some people recover full functional capacity even with a stage 2 uterine prolapse, so it is important to measure progress by their ability to live a full life, as they define it.
Implications of Uterine Prolapse on Sexual Function
There are many reasons why your patients might find that their ability to enjoy sexual intercourse is impaired by their prolapse. The bulging or intrusion of the uterus into the vagina can create pain and discomfort during penetration of any kind. Feeling like “something’s in the way” can be uncomfortable for both partners, and can lower satisfaction and ability to orgasm. The constant feeling of pelvic pressure and pain can have a negative effect on libido, potentially leading to avoidance of sexual activity.
In addition to the physical discomfort, your patients are likely suffering from self-esteem and body image issues stemming from feeling like their bodies are broken, which can also lead to decreased sexual desire. And of course, fear of making the condition worse can create anxiety around all kinds of activity, including sex.
Best Practices for Managing Discomfort During Intercourse
Because sexual desire and intercourse are not merely physical experiences, your patients will need a multi-pronged approach to managing their prolapse symptoms and maintaining or regaining satisfying sexual function. Mental health support should be encouraged throughout the healing process.
At the same time, there are evidence-based strategies for reducing discomfort during intercourse, including optimal sexual positions and generous application of lubrication. In general, since pelvic organ prolapse (POP) is an intra-abdominal pressure problem, positions that reduce that pressure can be useful, for example, lifting the pelvis with a pillow in missionary position, side-lying, or with the person with vaginal anatomy on top. Some ring pessaries without a membrane can be worn during intercourse; if your client has been prescribed a pessary, you might recommend that they talk to their doctor about whether the pessary can make intercourse more comfortable.

Treatment and Management Options
Managing uterine prolapse can take several forms. Unless the prolapse is so severe as to require emergency measures, most practitioners begin with more conservative treatments like pelvic floor physical therapy (PFPT) before introducing more invasive measures, like surgery.
PFPT will help address the movement patterns that can increase intra-abdominal pressure, which is a major factor in prolapse cases. For many patients, working with a PT and supplementing that work with a program like Restore Your Core® can fully resolve their symptoms within a year. Adding a pessary to their recovery program can help some patients progress with less physical discomfort. Some people find that occasional pessary use continues long-term, while others can wean off of it as their bodies get stronger and more coordinated.
If conservative measures do not provide relief, several surgical options are available for uterine prolapse patients. Most recent studies of uterine prolapse and sexual function focus on these surgical options; in general, treatments that reduce prolapse symptoms also tend to improve sexual function and satisfaction. However, it’s crucial to prepare for and recover from surgery with a pelvic floor rehabilitation program, as surgery alone does not teach your client how to manage intra-abdominal pressure. Preparing for and recovering from the surgery with pelvic floor physical therapy is essential to long-term healing–surgery does not teach your client how to manage intra-abdominal pressure. Engaging in pelvic floor physical therapy is essential for long-term healing and reducing the risk of prolapse reoccurrence.
Counseling Patients on Emotional and Psychological Aspects
The psychological impacts of prolapse on patients’ sexual relationships can be profound. While your role may not be to provide emotional counsel, you can nevertheless create an environment that allows for open and supportive discussions about sexual health. A few tips:
- Ask open-ended questions–for example, “how has sexual intercourse in the last few months been affected by your symptoms?”
- Give your patient time to answer, and remind them that there are no right or wrong answers
- Validate their experience and feelings–you can do this by using phrases such as “it sounds like this has been very difficult” or “it makes sense that you find this distressing.”
- Thank them for sharing their experience
You may also want to refer your patient to a therapist or other mental health practitioner; again, there are ways to do this without making your client feel broken. It’s incredibly common for a diagnosis like uterine prolapse to feel devastating since it can affect multiple areas of a person’s life. Referrals to counseling should be made frequently and without shaming.
Key Considerations about Intercourse and Prolapse
The most important thing you can do as a professional working with patients who have uterine prolapse is be both realistic and hopeful. Sexuality is an important part of a full life for most people, so acknowledging the grief that your patients may be experiencing with a change in their physical ability to have intercourse is essential. Patient-centered communication is key–what are your clients’ concerns? What do they consider a robust, thriving life? How achievable is that goal, given their condition? So often, patients receive a diagnosis like POP without understanding that while it is likely to be chronic, it can be managed, and many of their symptoms can be improved, if not resolved completely. Make sure that your patients are aware of all of their options, and that they can choose multiple routes toward healing.
FAQ
1. How do different types of prolapse affect sexual function?
Prolapse can cause discomfort, decreased sensation, pain during intercourse, and changes in vaginal anatomy, all of which can negatively affect sexual function.
2. What are the key factors to consider before recommending surgical intervention for prolapse in sexually active patients?
Factors include the severity of symptoms, the impact on sexual function, the patient’s age, overall health, and desire for future sexual activity, as well as alternative treatment options.
3. What immediate steps should be taken if a patient experiences discomfort during intercourse due to prolapse?
They should stop intercourse, consult a healthcare provider, and consider using lubrication, pelvic floor exercises, or a pessary to alleviate discomfort.
4. Can sexual activity worsen a prolapsed uterus, and how can this be prevented?
Sexual activity generally doesn’t worsen prolapse if done gently, but avoiding positions that cause discomfort and engaging in pelvic floor exercises can help prevent worsening.
5. How can professionals differentiate between symptoms caused by prolapse and other potential gynecological issues during intercourse?
A thorough pelvic exam, patient history, and sometimes imaging studies can help distinguish prolapse from other conditions like endometriosis or infections.
6. What advice can be given to partners of patients with a prolapsed uterus to support a healthy sexual relationship?
Encourage open communication, be patient and understanding, explore comfortable positions, and consider seeking guidance from a healthcare professional together.



