Pelvic Floor Therapy | Improving Your Pelvic Health
4 Min Read
Pelvic floor therapy is recommended for conditions where the pelvic floor and core system is not functioning optimally. Pelvic Floor Dysfunction and its related conditions can be caused by many different things. These can include:
- Infections
- Irritable bowel syndrome
- Pregnancy or childbirth
- Poor posture
- Trauma
- Chronic back pain
- Medical history of trauma, injuries in the pelvic region
- Surgery
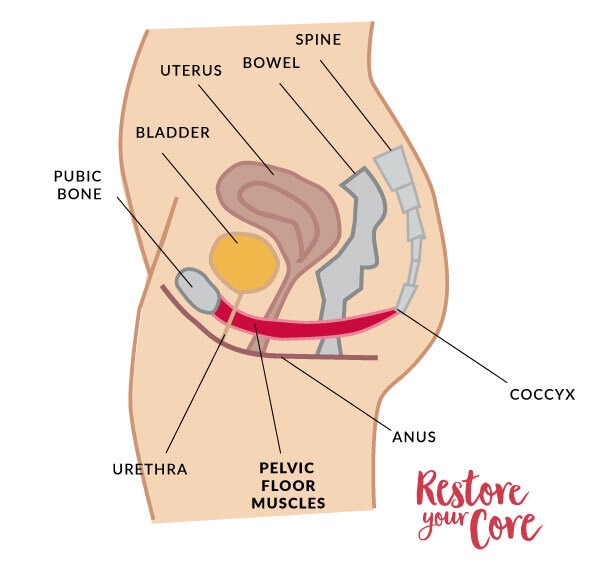
However, PFD can also seem to have no cause and present itself with a host of painful symptoms. In some women, the cause of PFD can be a result of postpartum diastasis recti. The pelvic floor is made up of muscles and other tissues which form a sling from the pubic symphysis to the tailbone. Many cases of PFD stem from a lack of sufficient support from the pelvic floor. These pelvic floor muscles assist in maintaining correct posture, abdominal and pelvic organ support, and aid in bladder and bowel control as well as sexual activity. If these muscles become overactive or overused (hypertonic), the results can be quite painful and function can decrease significantly. Less often, the pelvic floor muscles are hypotonic–lacking sufficient resting tension to perform their jobs. Yet, due to the complexity of the anatomy and functions of the pelvic region, the underlying cause of pain can be difficult to determine. In this case, the whole body must be treated and physical therapy including pelvic floor exercise can greatly aid in men and women in their healing process and recovery.
Table of Contents
Why do I need pelvic floor therapy?
(POP) or pelvic organ prolapse is a type of pelvic floor dysfunction in which one or more pelvic floor organs (i.e. bladder, rectum, small bowel, uterus, etc) shift toward or down into the vaginal canal. This most commonly happens with conditions like diastasis recti, which create an imbalance of muscle and ligament tension supporting the pelvic floor; many people who have POP also have a DRA. Women who experience a pelvic organ prolapse sometimes describe the occurrence as feeling like a “stuck tampon,” a heavy pelvic floor, or as bubbles in the urethra. Some other pelvic floor dysfunction symptoms may include:
- constipation
- pelvic pain during sex
- experience pain during intercourse
- painful ejaculation (in men)
- urinary symptoms
- urinary/bowel incontinence
- rectal pain
- sharp shooting pain in the lower back
- painful urination, difficulty with urination
Most fitness gurus try to educate their clients with core exercise routines that engage the pelvic floor and the core together. They believe that if you engage your core in any activity, you should also engage your pelvic floor. However, I believe there is a lot wrong with this routine and practice.
As a trained and educated professional, I never, ever attempt to teach pelvic floor muscles to engage in exercise. Rather, it is important to train the pelvic floor to lift and release appropriately depending on the exercise and the weight. This is what I teach in my 13-week program, Restore Your Core.
What do they do in pelvic floor physical therapy?
In physical therapy for pelvic floor issues rehabilitation may vary. An initial assessment will most likely be made by your physical therapist. This can include a manual therapy or palpation either vaginally or rectally. Palpitation of the vaginal wall helps physical therapists determine muscles tightness, areas of tenderness and pain, and muscle strength.
Getting to Know Your Pelvic Floor

Imbalances of the pelvic muscles – can be difficult to feel and perceive. One of the most unhelpful tips that pelvic floor exercisers tend to give is the misguided and incessant demand for exercising kegels. Kegels can prevent treatment from happening because it creates tight muscles, increases muscle tone, and may contribute to muscle imbalance, which makes your pelvic muscles even harder to feel. While Kegel exercises performed correctly can be useful for toning the pelvic floor muscles, in the case of hypertonic muscles, you’re adding tension to tension, and not actually increasing the responsiveness of the muscles – and in this case making your pelvic floor muscle dysfunction worse and may experience physical pain as a result. As a result, doing 100 Kegels a day may actually make your symptoms worse; increasing the tension in the pelvic floor muscles can also make it harder to perceive the movement of the pelvic floor.
One of the key elements of the healing process is awareness. When you are aware of the structure of your body and whether or not it is performing correctly, you can begin resolving your problems. If you are blind to it, you may continue to practice bad habits due to motor programming. However, if we want to shift things around in order to eliminate physical pain and encourage realignment, we must shift our habits as well.
In the case of POP or other pelvic floor issues, there can be a lot of confusion. Some of the most common questions I get asked are:
- Is my pelvic floor too tight or not tight enough?
- How can I tell if I’m practicing resting tension?
- How can I fix this?
Before we can begin resolving any present issues, we have to get to know our pelvic floor a bit.
We must understand various aspects of physical therapy techniques. This means that we need to understand what it means to engage the pelvic floor, what it feels like to release and contract, and how to both control contractions and release. Only then can we properly discern what unhealthy tendencies we may fall into. At first, many women find that they have little to no control over their muscles. Over time and with practice, this often changes.
Reduce Intra Abdominal Pressure: Breathing Mechanics Matter
One of the key pieces of pelvic floor rehabilitation is breathing mechanics. In Restore Your Core, I spend a great deal of time with my clients teaching them proper breathing mechanics. How you breathe has a significant impact on the integrity of your core and pelvic floor. However, many of us do not even realize how easy it is for us to fall into incorrect breathing patterns.
Many people are belly breathers. This means that every time they inhale their bellies inflate. Think of it this way: if you were to fill an oval-shaped balloon with water and then squeeze the top, what would happen? It would bulge! The same thing happens when we belly breathe. When the bulge happens, you’re straining your core and pelvic floor with an excessive amount of pressure. This can damage the muscles and organs in that region. Our PF is not designed to handle a great deal of stress and pressure.What I teach my clients instead is a technique called 3D breathing. This breathing method engages the rib cage and the diaphragm. When you inhale, your ribs expand instead of your belly. Breathing this way reduces excessive intraabdominal pressure.In fact, this technique promotes proper core engagement and response in your daily activities. Pelvic floor issues go hand-in-hand with core function–when you’re looking to resolve pelvic floor dysfunction, you will also address core dysfunction.Check out this video I made discussing the connection between belly breathing and pelvic floor/ core issues and how to properly re-train your breath.
Reduce Intra Abdominal Pressure: Alignment Matters
Daily movement habits and activities can greatly affect the health of our pelvic floor as well as our joints, muscles, and bones. When I work with my clients with POP or PFD, I always want to ensure their pelvic alignment is optimal. Without even realizing it, many people end up standing and pushing their hips forward. This shift can greatly affect the effectiveness of the core muscles. Treatment for pelvic floor restoration should include educated instruction on correct posture and relaxation exercises.

How you stand can greatly affect your body over time. Muscles holding your alignment in place can shift and move to accommodate habitual stances and movements. To stand correctly, stand up straight and tall. Focus your weight on the balls of your heels and level your feet with your shoulders, knees bent. Next, relax your arms at your side. Keep your head straight and level (earlobes aligned with shoulders) and pull your shoulders back. If you’re standing for long periods of time, shift your weight from your toes to your heels.
Restore Your Pelvic Floor and Core: Exercises
Now that you are better versed in breathing, alignment, and got to know your pelvic floor, you should begin holistic exercise and movement to strengthen and integrate your pelvic floor & core. Some of the benefits of physical therapy programs include:
Pelvic Floor Therapy can help with:
- incontinence
- difficulty with bladder or bowel movements
- painful sex
- constipation
- pelvic pain
- endometriosis
- vaginismus
- menopause symptoms
- pregnancy and postpartum wellness
As you know by now, PT goes way beyond kegels. My 13 Week Program: Restore Your Core offers a step by step approach to strengthening your pelvic floor and whole body. If you feel a bit unprepared to tackle a long program, here is a video of 5 exercises that are wonderful to get you started. If you have discovered imbalances in your pelvic floor, you might also reach out to a pelvic health physical therapist near you.

How long does it take for pelvic floor therapy to work?
This depends on the severity of the issues at hand. However, there are many things you can begin doing now to help begin the healing process.
Healing can take anywhere from a few months to over a year, depending on whether or not there are underlying conditions which may be increasing the pain. While there are no overnight success stories, there are many, many success stories of women like you who have healed their pelvic organ prolapse and increased their quality of life by taking these steps slowly and surely.



